It started with a thread about infant feeding that the lovely Lucy began on the #MatExp Facebook group. It was a fantastic discussion with a realistic and compassionate look at all kinds of barriers and problems, but one comment from student midwife Amy Prodgers stood out for me the most:
“Have found this discussion really fascinating as have been reflecting on similar issues after my first week on postnatal ward as a student midwife. I could go on about loads of things but a key point for me is the conflict between safe sleeping advice and facilitating breastfeeding. Women are exhausted from their birth experiences and their babies just want to feed but can’t sleep together. Women then end up feeling a failure for not being able to settle their babies in the cot, whilst also feeling guilty for wanting to sleep. This is when women start asking for formula and when midwives begin to doubt their intentions. Totally undermines confidence.”
I started a new thread with this comment at the top, and tagged in Gill Phillips as I felt it would make an excellent scenario for the WhoseShoes game that is used in #MatExp workshops around the country. We then had a discussion about bedsharing that raised some important points, and I felt it important to capture that discussion and share with you here.

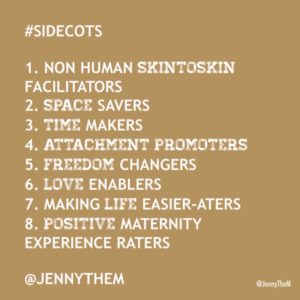
What was quickly brought up was the co-sleeper cots that used to be available to women on some postnatal wards. This article was linked to: http://www.scarymommy.com/hospitals-everywhere-should-have-this-amazing-co-sleeping-bed-for-new-moms/ and I remembered that midwife Jenny Clarke had been tweeting about them this year.
An IBCLC on the group explained that “The old co-sleeper cots don’t fit the new beds (which were needed to reduce back strain on staff). However there are several new designs that fit the new bed, and research starting up too. Helen Ball’s research and videos of mothers clearly showed that the co sleeper cots made things *much* easier for mothers, much happier for babies, and didn’t add to staff’s workload.”
But would co-sleeper cots solve the problem? A paediatric consultant commented “I had co-sleeper cots after both my deliveries but actually my babies just wanted skin-to-skin for the whole first night. I think we really need better hospital beds in maternity and children’s wards to facilitate bedsharing.”
The important thing to bear in mind here is that these babies are displaying completely normal behaviours. It is our maternity wards that need to be “fixed”, not the babies. For a lot more discussion about expectations and reality when it comes to infant sleep, please see this blog by Alice Amber-Keegan of the Infant Sleep Information Source: https://growingfamilies.co.uk/2016/09/04/infant-sleep-expectations-and-reality/
Founder of the Positive Birth Movement, Milli Hill, agreed that “co-sleeper cots imply that at some point your baby will not mind being put down separately from you, and that you won’t mind putting them down separately either! Not always what mum or baby wants or needs.”
And of course, not having baby on the same surface as you can make life very difficult for post-birth mothers, as Polly Rogerson pointed out: “I was in hospital for a week after birth [due to post-partum haemorrhage], I was so weak that I couldn’t even lift my baby out of the cot – even with it right next to the bed. Yet somehow I was expected to do exactly that to try to feed him.”
Bedsharing when Baby is Unwell
The conversation then went in a couple of different directions – one discussion of bedsharing on children’s wards when a baby is ill, and one discussion of the guidelines that trust’s expect health visitors to follow when discussing bedsharing with the families they support.
Anyone who follows my hospital breastfeeding campaign will know how excited I was to have a paediatric consultant say that it would be good to have bedsharing facilitated on children’s wards! The consultant in question went on to say:
“Because in real life, I’d say close to 100% of families bedshare when children are ill. Banning it on hospital wards is just stupid. Having informed discussion about it is sensible.”
She clarified that her reservation for bedsharing with unwell children “is smoking parents and small babies and children with respiratory illness, as it is unrealistic to expect parents to stop smoking at such a stressful time, but the smoke clinging to clothes and hair definitely seems to exacerbate the children’s respiratory problems.” However this doctor confirmed:
“I spend a lot of time at work putting babies and children back into parents’ arms. That’s where they are usually happiest, but most importantly for me, most physiologically stable!”
This issue came up on my own private Facebook group today, as a member explained that her niece was hospitalised (and will likely be so for some time) and is refusing to sleep anywhere but on mum. As mum is unable to bedshare in hospital due to lack of facilities, mum is getting very little sleep.
A paediatric nurse on my group explained that from her professional perspective “we never advocate or advise co sleeping in our hospital as the babies are with us due to illness & therefore it can increase the chances of problems. However it is a parent’s choice and some still do, but we are bound by our duty of care to highlight the implications.”
She went on to say though:
“I’m a big believer in family centred care (which all children’s wards/nurses/professionals should be) so if a parent still wants to co sleep (and they would do so at home) I feel it’s my duty to help that parent as best I can so their wishes are upheld, but in a way that I feel most comfortable with in my work setting. As a children’s nurse you’re not only nursing the child but the whole family too, so to keep things as they would do at home or in regular life is important; the change of circumstance by being in hospital is bad enough for the child and family never mind then saying ‘well sorry you can’t keep your normal routine whilst here’. I think sometimes as a health professional we’re so focused on making that child better medically it can be forgotten how big a change being in hospital can be on them emotionally; even though they may not outwardly show signs of distress it is definitely affecting them psychologically, and therefore keeping things as much to their norm as possible is very important.”
Bedsharing when Baby is at Home

The discussion about what health visitors can and can’t say to new parents was prompted by one mother explaining “my health visitor at 6 weeks (1st baby) gave me info about safe co-sleeping and it was the reason I continued to breastfeed.”
I then shared the discussions that mothers from my group have had with health visitors online, including a discussion specifically about bedsharing: HVe-COP newsletter The two quotes from that discussion that summarise the issues for me are:
“We are very constrained sometimes. We have to follow Trust policy…..even if we believe that bed sharing can be very beneficial and are up to date (with evidence)” (health visitor participator)
“Just to put this out there…….we have a responsibility to our NMC Code of Practice and the clients…after that Trust policy is important. The day health visitors do not provide evidence based information to their clients because of Trust policy is a grave one indeed” (health visitor participator)
On this thread in the #MatExp group, one health visitor explained: “Trust guidance is the Lullaby Trust safe sleep recommendations, and signposting to NICE for bed sharing…..personally I don’t advocate it but I talk about if [you are] bedsharing [how to] minimise risks.”
This conversation took place before the launch of the new Baby Friendly “Co-sleeping and SIDS” guidance for healthcare professionals, which has been developed in conjunction with the Infant Sleep Information Source and the Lullaby Trust. This guidance focuses on helping healthcare professionals “to take a sensible, proportionate parent-centred approach in order to find practical solutions to this complex issue”.
We can hope that this guidance and the continued expansion of Baby Friendly training for UK health visitors will put an end to less nuanced campaigns such as this one from Bolton, Wigan and Salford that Amy Prodgers highlighted:
As you can imagine, this heavy handed campaign elicited a strong response from those on the thread! Amy herself commented that “reducing SIDS by telling people not to bed share is a bit like reducing road traffic accidents by telling people not to use cars! And of course we’ll also avoid the issue of how much more dangerous it is to fall asleep on the sofa (whilst presumably trying your best to follow this advice and stay awake).”
One mother’s experience explains the reality of what happens when health visitors advise against bedsharing: “When I told my HV I was co-sleeping, on purpose and in accordance with safety instructions, she gave me leaflets on ‘cot death’ and strongly discouraged me from doing it. She then arranged another visit for a few weeks later, after advising me to ‘keep trying with the moses basket’. When she returned I just lied and said that my baby was now sleeping in the basket as I couldn’t be arsed with having to defend my conscientious parenting decisions.”
For information on the practicalities of sharing a bed with your baby, please see this detailed post by Elena Abell: https://growingfamilies.co.uk/2016/06/15/the-practicalities-of-sharing-a-bed-with-your-baby/
Or see the “Safe Sleep Seven” from La Leche League:
And for the latest research on bedsharing, infant sleep and SIDS please see the Baby Friendly website: https://www.unicef.org.uk/babyfriendly/news-and-research/baby-friendly-research/infant-health-research/infant-health-research-bed-sharing-infant-sleep-and-sids/
Midwife Sally Goodwin said at the end of the thread that she was “grateful to all for highlighting this issue. I think this subject comes up erm…… every day for me as a midwife.”
Certainly a topic we need to continue to discuss then.
Helen Calvert
November 2016