We are very honoured to begin #ExpOfCare week with a bang, publishing this insightful blog by Dr Sarah Winfield. We have connected with Sarah through the excellent ongoing #MatExp work at Leeds Teaching Hospitals NHS Trust, following the exciting Whose Shoes? workshop last summer. Part of the work in Leeds involves a different #MatExp challenge each month… and January 2017 was ‘lithotomy challenge’ month!
Sarah wrote this a while ago but we held it back to publish here as #ExpOfCare is such an important initiative and one which is central to #MatExp. We are very grateful to Sarah not only for taking the time to do the challenge, but more importantly to reflect so openly on the experience and share with us here…
The #LithotomyChallenge is a term coined by one of my Obstetric colleagues in Kingston, Dr Flo Wilcock, who wanted to put herself in the position of a patient in lithotomy for an hour and to describe the experience. As part of #MatExp and to raise awareness of it’s existence and philosophy, I wanted to do the same. So I did on #NHSDoAthonDay at the start of January 2017. Here is how I got started.
I used to be sceptical about twitter until my tech-loving husband persuaded me to dust the cobwebs off my twitter account @winners352 (set up tentatively a while ago). David is a consultant in Education and assured me that performing CPR on my twitter account would not only be beneficial for my CPD, but would put me in touch with like-minded people, allow me to tweet the odd journal article, and would help me to raise the profile of the unit that I work in. I wasn’t ‘sold’ but I am an optimist and thought that I should give it a go.
So I changed my profile picture, tried to compose a sassy yet professional catch line and I started to browse for people and things that may interest me. Initially I retweeted posts that would not cause any controversy for my digital footprint or reputation as a member of the medical community, but then I worked out that if people put their opinions out there for all to see, then this provokes engagement and discussion. This conversation would then draw others in. Then information begins to flow, more people ‘follow’ and before you know it, there are people from all over the world tapping in to see what this is all about. Amazing. But also slightly scary.
Of course, I appreciate that there are downsides to having a twitter presence, but this is where the world is going now. I recall an article written for the Health Service Journal by Roy Lilley about STPs (Sustainability Transformation Plans). In this article, to paraphrase, he said that STPs are happening and are not going away, so you can be in the cast or the audience. It’s your choice. I think that the same applies to social media and twitter. So, I made the decision to learn more and make it work for me. This was at the beginning of October 2016.
Through twitter I made contact with Gill Phillips (@WhoseShoes) and Flo Wilcock (@FWmaternitykhft) who are the founders of #MatExp, and it turned out that I had actually met one of this duo before!
As well as being a Consultant Obstetrician with an interest in maternal medicine, I am also the Clinical Lead for maternity services for the Yorkshire and the Humber Clinical Network. This role took me to an event at the Kia Oval in London in July 2016 to discuss implementation of ‘Better Births’ (the National Maternity Review) in each network patch. There were a series of workshops and in one I joined in with a discussion about the “Whose Shoes” event that had been held in Leeds earlier in the year. I did not realise it at the time (probably because I was not on twitter at that point!) but Gill Phillips was one of the facilitators of that group. Professor Cathy Warwick and Mr David Richmond were the other facilitators.
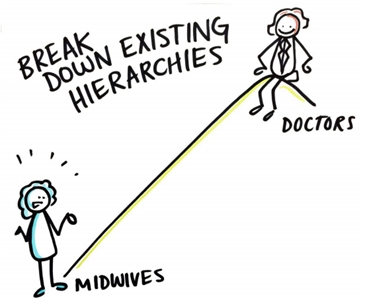
While I had not been able to attend the Leeds Whose Shoes event itself, our LTHT strategy midwife, Sarah Bennett, was very much involved. At the event a cartoonist, Tom Bailey, recorded patients’ views and the conversations taking place. These were very thought provoking and I have to admit that one image in particular made me stop and think. It was of a doctor standing at the top of a hill pointing down to a midwife at the bottom of the hill. It was not particularly complimentary to us as doctors.
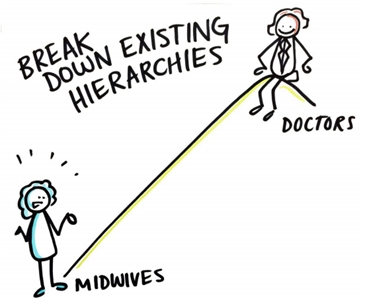 None of us set out to make patients and midwives feel like this but with the language we use, the information we need to get across and our communication skills in general, there was clearly an issue. This made me feel uncomfortable (and perhaps a tad indignant, if I am being honest) and I know that a few of my colleagues felt the same as me.
None of us set out to make patients and midwives feel like this but with the language we use, the information we need to get across and our communication skills in general, there was clearly an issue. This made me feel uncomfortable (and perhaps a tad indignant, if I am being honest) and I know that a few of my colleagues felt the same as me.
What happened though was that these images stimulated discussion and debate amongst the maternity staff members. While there might have been levels of disagreement about the images and what they portrayed us to be as medical and midwifery professionals, they were ‘real’ views of and we had to reflect here. Importantly these conversations were a starting point to encourage us to look at how we work on a day-today basis, the language we use with patients and each other, how we conduct ward rounds on the delivery suite and the whole experience for any woman and her family using our maternity service.
In other words, we had a platform from which to share our opinions about the maternity experience of patients in Leeds across both sides of the city.
Leeds is a busy tertiary unit. We have around over 10,000 deliveries a year between Leeds General Infirmary (LGI) and St James’s Hospital (SJUH) and we don’t often get to do sit down with our colleagues, whose opinions we genuinely value, and engage in a dialogue about patient experience. But here we were, and I felt like this was a good start.
I spoke about this experience in positive terms at the Kia event and Gill then made contact with me through twitter a few months later. A fortuitous connection for me and, I hope, for her too. I also ‘met’ Flo through Gill on twitter, and the rest has followed.
So who are Gill and Flo and what is #MatExp?
Gill, the creator of the award-winning Whose Shoes?® concept and tools, has a genuine passion and unsurpassed energy for “looking at issues from different perspectives and getting people to talk together as equals and come up with imaginative solutions”. She is also a mum of three ‘now grown up’ children.
Her website http://nutshellcomms.co.uk/gill-phillips-and-the-origins-of-whose-shoes/ is an inspirational working ode to her warm, inclusive and collaborative style. Gill’s passion for helping others is obvious to see and she takes people with her. This is one of the many reasons why she has been quoted by the Health Service Journal as one of the 50 most influential women of the year.
Florence (Flo) Wilcock is a Consultant Obstetrician at Kingston (and mum of two) and, inspired by Gill’s WhoseShoes concept, was keen to use this to improve maternity services and more. Flo is similarly an inspirational force and counts the RCOG and its former president David Richmond as her supporters, amongst many others. She joined forces with Gill and the #MatExp campaign was born.
The #MatExp website is a vibrant, colourful, positive and proactive resource and I would advise anyone working with women and their families. The best explanation of #MatExp is the one from their website, so in their own words:
“#MatExp is a powerful grassroots campaign using the Whose Shoes?® approach to identify and share best practice across the nation’s maternity services.
Then ensued a flurry of tweets between me, Gill, Flo and other #MatExp supporters and I was overwhelmed by the helpful, collaborative and go-getting approach. They are incredibly supportive to anyone on twitter who shows an interest in improving patient and family experience in maternity services.
As my knowledge grew about #MatExp and I had further twitter conversations with Gill, Flo and others, I read a piece by Flo that she wrote about her taking part in a #Lithotomychallenge. The piece is here and Flo explains:
“For NHS change day I wanted something that made a statement that said “#MatExp has arrived, take notice, we are improving maternity experience, get involved!” I couldn’t quite think of the right action until I saw a twitter exchange with Damian Roland back in December and watched a video where he described his spinal board challenge from NHS Change day, 2014. I had a light bulb moment thinking what would be the maternity equivalent? Lithotomy!”
Taking Flo’s lead and transporting #MatExp to Leeds, I thought that a #LithotomyChallenge would be easy for me to set up and would put me in a patient’s shoes (goodness knows the amount of times in my career that I have put a patient in the lithotomy position for an instrumental delivery, a FBS, a perineal repair..) for a short while. I have two daughters, both born by caesarean section, so I had no experience of this, let alone with contractions, CTG leads, an epidural, a syntocinon drip etc.
I chose Wednesday 11 January 2017 as the morning I would do it. This was #NHSDoAthonDay and it seemed appropriate.
In the run up to the day, Sarah and I told people what I was going to do through the strategy newsletter, facebook, twitter and word of mouth. People asked why and asked what #MatExp was. There was also an interesting spectrum of opinion about my desire to do the #Lithotomy Challenge, ranging from people thinking that I was ‘patronising’ my patients and colleagues to others congratulating me for taking the initiative to do something different.
 On the day of the challenge I put my hospital gown on, strapped the CTG leads to my abdomen and Sarah fixed an IV line to hand with tape and helped me up onto the delivery bed in Room 10 on LGI delivery suite. Then Sarah left to go across the city to St.James’ hospital where the midwives there were waiting for her to set them up with the #Lithotomychallenge too. I was by myself in the room. In lithotomy position.
On the day of the challenge I put my hospital gown on, strapped the CTG leads to my abdomen and Sarah fixed an IV line to hand with tape and helped me up onto the delivery bed in Room 10 on LGI delivery suite. Then Sarah left to go across the city to St.James’ hospital where the midwives there were waiting for her to set them up with the #Lithotomychallenge too. I was by myself in the room. In lithotomy position.
I felt undignified and vulnerable. I also hoped that nobody would walk through the door, but they did. In groups, in pairs, alone. Mostly midwives. Each time I cringed as the door opened and I realised that the level of the bed meant that my bottom end was at their eye level. I was in leggings and a sheet. I can’t imagine the indignity and embarrassment for a woman of being ‘al fresco’ when someone comes into the room in that situation.
Then I noticed something that I hadn’t before; there was no ‘privacy curtain’ over the door. I now realise that this curtain is a feature of the delivery rooms at St.James’ hospital across the city and in every other maternity unit I can recall having worked in before. Such a simple thing would make a huge difference.
Then the surroundings really began to jump out at me. This room had magnolia walls, a light socket that was hanging off (previously an uplighter), holes and scuffs in the walls and nothing that I would describe as comforting, pleasant or homely. When you sit in a room for over an hour, these details are very obvious. I have been in this room many times during ward rounds, to deliver babies etc. and I had never noticed what an uninspiring and depressing environment it is.
Would I have enjoyed my birth experience in this room? Definitely not. Does it convey an impression of the warmth, skills, knowledge, team spirit and professionalism of the delivery suite staff that I know exists? No it does not. But a woman and her family have this room as the starting point on their personal, special and much anticipated journey to give birth to their precious baby so how is it going to set them up for a positive birth experience? It don’t think it will.
Then something unexpected happened. I felt really cross with this room, if it’s possible to be annoyed with a ‘space’. I know how hard the team work to look after women and their families, so why should the woman and us as the team, with our training, skills, compassion, knowledge and tertiary centre reputation be let down by awful facilities? All women should have a pleasant environment to have their baby. It’s very simple. Some paint, some wall décor, good lighting, promptly repaired faults. The list is not long and is easily addressed. This was the first unexpected result for me of my #Lithotomychallenge and I have to say that it really touched a nerve.
The other unexpected result for me what that when people came in to see me they shared their own birth experiences (good and bad) as I sat there on the bed
with my legs ‘akimbo’. I found this moving because these are people who I have worked with for the last few years, who I chat with when I’m on-call and who I think I know quite well. I heard stories of a fantastic waterbirth, an awful induction, someone struggling to get pregnant plus more. You could say that the ‘barriers’ were down, but I would like to think that me doing this challenge provided an opportunity for people to start conversations with me and each other about their experiences as patients in the maternity service.
My final recollection added some humour to my experience. While I was talking to a group of student midwives (they appeared to be more embarrassed than me), one of our delivery suite domestic staff, who I know quite well, knocked on the door, walked in politely and without ceremony, gave me a glass of water and asked me for the keys to my office so that she could give it a clean while I was tied up! There was no pulling the wool over her eyes. I gave her the key and my thanks.
So, what did I get out of doing the #Lithotomy challenge? There are two things that stand out for me. The first is that I allowed myself to ‘feel’ from a patient’s perspective. I was prepared to give a bit of myself away and open up to the possibility that we may not communicate in a way that enhances a patient experience or consider the importance of the environment that we create to do this. I think that to change culture, the language we use and the way we view the patient experience we need to look closely at our individual practice and challenge our own behaviours and judgements. This is hard and not everyone will want to do this but I have found that doing the #LithotomyChallenge has led me to review my own beliefs and practices as an NHS worker for almost 20 years and this has been like taking a deep breath of fresh air.
As a doctor and a consultant I am familiar with pushing my boundaries professionally and clinically, but can I use any ‘influence’ that I have in a different way? Of course I can be an ‘opinion’, counsel patients, make management plans, perform difficult c-sections, chair regional meetings etc. but working towards improving patient experience may be regarded by some as a ‘fluffy’ goal. Very ‘touchy feely’ and not really hard-hitting or go-getting enough to warrant using precious consultant time in an already busy day where we are here to deliver a service and fulfill the objectives of our job plan/appraisal personal development portfolio. But sometimes it’s not until you experience the ‘other side’ and and allow yourself to ‘feel’, that you realise what needs to change. I now know that I would like to be more proactive in considering the whole patient experience when I am involved in any aspect of a consultation or a procedure.
The décor was the second thing. I have seen many articles and personal commentaries about the effect of surroundings on birth experience, and we already know that the environment during labour and delivery can have a profound effect on how patients ‘experience’ their care. After spending time in a room that has seen better days, I can believe it. Never underestimate the importance of surroundings and this challenge has highlighted that for me. I hope that this piece will result in privacy curtains being put up in each delivery room at LGI. This would make such a difference. But improving the delivery rooms in this unit is going to require funds. I regularly see healthcare workers and patients fundraising for their units and doing the #Lithotomychallenge to spurred me on to do this.
There is one final thing that the challenge has done. By writing this piece I have a voice. I have not asked permission and have not sought the ‘approval’ of anyone. I have just done it and have been supported by most of my colleagues, including Sarah B. I was nervous about doing the #LithotomyChallenge and had a sense of trepidation about what others would think, but I have enjoyed what the experience has brought and have been inspired by Flo and Gill, who have given me a masterclass in wholeheartedly and warmly welcoming others thoughts and diverse opinions. In their eyes no opinion is ‘wrong’ or ‘daft’. If disagreement arises then it is not to be feared or ridiculed. It can be used as the basis of a conversation to challenge the status quo and then move forwards.
“Change will not come if we wait for some other person or some other time. We are the ones we’ve been waiting for. We are the change that we seek” (Barack Obama).
Dr Sarah Winfield
Consultant in Obstetrics with Special Interest in Maternal Medicine. Leeds Teaching Hospitals NHS Trust
Yorkshire and the Humber Clinical Network Clinical Lead for Maternity Services
NHS England Women’s Specialised Services Clinical Reference Group representative for the North of England