There have been some fantastic conversations taking place on the MatExp Facebook group, with lots of ACTION threads being posted to generate discussion. The aim of these discussions is to identify ways that we can ACT to improve maternity experiences. Big, long-term actions that might require system change or a change in culture. And small, immediate actions, that professionals and individuals can take today to improve the maternity experience of those around them.
Over the last six months two big themes have emerged from #MatExp for me. The first is WHY are so many age-old issues still a problem for maternity care in this country? The answer to me is the working environment midwives face, as discussed here. The second is HOW can we make a real difference to family’s maternity experiences? So many actions have come out of #MatExp but the one that stands head and shoulders above, in my opinion, is continuity of care.
I don’t mean Ed Milliband’s diluted version of “the same midwife throughout labour”. I mean the same midwife antenatally, during labour and postnatally, or the same team of two or three midwives for the whole of that period. Women who hire independent midwives or who have access to OnetoOne Midwives have this type of continuity antenatally and postnatally, but they only have those same midwives during labour if they give birth at home. IMs and OnetoOne are not insured to act as midwives in hospital settings, although they can accompany women to hospital as advocates. Doulas are also with women as advocates and support for the whole of their pregnancy, birth and postnatal period but they are not qualified to act as midwives.
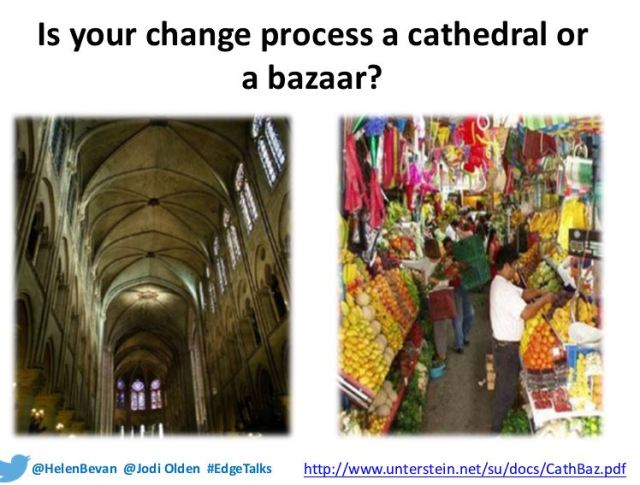
When I brought up continuity of care as an ACTION thread on Facebook, I asked the following questions:
- What are the barriers to providing continuity of care on the NHS? Is it as simple as not enough midwives, or is there more to it than that?
- As an anxious person I really prioritised continuity of care, so used an independent midwife in my first pregnancy and a OnetoOne midwife in my second. What would my options have been on the NHS, under what circumstances can women be put onto a one-to-one care pathway?
- What ACTION can we take to make continuity of care a reality?
- What ACTION can we take to build good relationships between women and their midwifery teams where continuity of care is NOT a reality?
The suggested actions from the discussion that followed were:
- Demonstrate the benefits of caseloading to NHS midwives
- Strong leaders at the helm of trusts who themselves understand how to implement and lead their midwives into wanting continuity of care
- NHS trusts to talk to independent midwives and social enterprise midwives who are the knowledgeable ones when it comes to providing continuity
- Think about options for a team approach. One group member directed us to look at the Streatham Valley midwife team: “They were part of a pilot scheme for community midwives where you saw the same midwife and often they came to you for booking in and later appointments. They also checked you at home when in labour to avoid wasted trips to hospital and they have an excellent home birth record. Out of my ante natal group of 5 first time mum’s none of us had anything stronger than gas and air we had one home birth and only one use of forceps. They are amazing.”
- Understand the positive impact that continuity of carer can have on patient safety and infant mortality
- Find ways to care for midwives and avoid the “burn out” that is often associated with a caseloading model of working
- Women with more complex pregnancies to be caseloaded by a team expert in their complexities – in other words, being at a higher risk of complications should not exclude women from continuity of care, in fact if anything these women need it more
- Consider personalised budgets ( i.e. the NHS would allocate a woman funding to choose the service they wish) and whether or not this concept could help in delivering continuity of care
- If continuity is not available then note-keeping needs to be excellent so women don’t always have to repeat themselves (which can be particularly hard following baby loss), and so that plans can be discussed and followed up
- Women who are vulnerable or at risk of perinatal mental health problems should be at the front of the queue for continuity of care
- Ensure that families are aware of and understand any choices they do have when it comes to their maternity care team
One healthcare professional commented “The commonest refrain you hear from mothers these days is ‘I never saw the same midwife twice’; this is a great sadness to me as surely the greatest gift to mediate the stressful vocation that is midwifery, is the relationship you develop with your ladies.”
Another woman who had opted for independent midwifery care in her second pregnancy commented “I just needed to know that someone was going to know me personally and take my wishes/needs seriously.”
Continuity of care was the strongest theme in the feedback to the National Maternity Review provided by my private Facebook group. It comes up time and again in discussions – I was discussing it today with student midwives at Salford University and they agreed that many midwives want to work to a caseloading model as much as families do. It just has to be constructed in a way that makes it feasible for midwives, many of whom have young families themselves.

This is not news. The RCM’s Better Births campaign has continuity of care as one of its key themes. The demand for caseloading from families accounts for the popularity of OnetoOne midwives in the areas where they are commissioned. A group of mothers in Greater Manchester is campaigning for the local CCGs to make this service available to women, and as someone who has benefited from that company’s care I joined them on a demonstration in Manchester city centre. If continuity is not going to be available on the NHS then OnetoOne might be the best option for families, although as this post of mine shows not all women find that the various services work together.
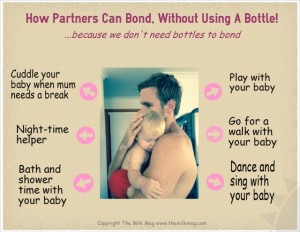
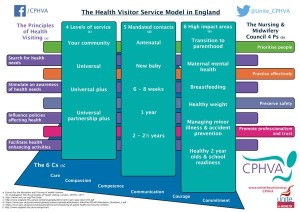
What I find striking is how much continuity of care would impact on other areas where the #MatExp campaign has asked for ACTION. Anxiety is reduced if women know their carers. Emotional well-being is improved as are infant feeding outcomes. Dads & partners have more chance of being involved and having their own struggles recognised if they are able to get to know the family’s care team. It will be far easier for midwives and health visitors to collaborate if it is clear who is looking after which families.
I was delighted when an insurance solution was found for independent midwifery in this country. I also have high praise for the model of care provided by OnetoOne. Support and advocacy from a doula can be invaluable. But continuity of care should not be on the periphery of the UK maternity experience. It should BE the UK maternity experience.
Helen Calvert
@heartmummy
2015




 via http://www.pantley.com/elizabeth/%5B/caption%5D
via http://www.pantley.com/elizabeth/%5B/caption%5D