I am delighted to be able to publish today a guest blog for the #MatExp campaign from Mr Raja Gangopadhyay. Raja is a Consultant Obstetrician and Gynaecologist with special area of clinical interest in Perinatal Mental Health (PMH) from West Hertfordshire Hospitals NHS Trust. He is a member of the Royal College of Obstetrician and Gynaecologist (RCOG).
I would like to take this opportunity to share my views on why I feel so strongly about the role of the Maternity Services in Perinatal Mental Health (PMH).
Perinatal Mental Health (PMH) has two important components in its terminology: ‘Perinatal’ (period during pregnancy, delivery and post delivery) and ‘Mental Health’. Therefore the care of mums in the Maternity Services during this vital period is of utmost importance in PMH: it should be a no-brainer.
But sadly, PMH is the only one area of Maternal Health where I do not see a strong voice of the Maternity Services in the national campaign.
This has remained ‘Cinderella’ within Maternity Units in spite of the glaring facts:
-
PMH is still one of the leading causes of maternal death in the UK.
-
This is one of the most prevalent conditions mums suffer from during their pregnancy and postpartum period (at least 10% of mums suffering from this).
I strongly believe that without robust ‘perinatal’ care, women would continue to suffer and die from PMH illnesses, no matter how much we spend to expand specialist Mother and Baby Units (MBUs).
Therefore this is the time when we must recognise this important area and raise awareness.
I am trying to address this issue through my campaign on social media and as the Royal College of Obstetrician and Gynaecologist’s (RCOG) Representative to the Maternal Mental Health Alliance (MMHA).
What do I mean by PMH ‘within’ Maternity Services?
Suffering and deaths from PMH illnesses are often preventable if appropriate measures are taken during pregnancy and in the immediate postpartum period.
A prevalent health condition like PMH must be managed with the same readiness as managing other medical conditions in pregnancy such as diabetes, high blood pressure (pre-eclampsia) or heart disease.
The only way to ensure that the women with PMH are appropriately cared for according to the NICE guideline (2014) is to have:
-
A dedicated PMH team within every Maternity Service:
A Consultant Obstetrician, Specialist Midwife, a Perinatal Psychiatrist, a Specialist Psychiatry Nurse and a Paediatrician should jointly lead this service locally. The service should be easily accessible to the mums.
-
A dedicated Obstetric-Psychiatry Antenatal clinic
-
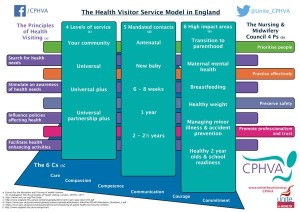
Communication with Community Team:
This Maternity Service should have clear links with GP, Health Visitor (HV), community MH Team, Liaison Psychiatry services, Mental Health Crisis Team, Children and Young People services, Peer Support groups and other charitable organisations.
-
Robust Care Pathway:
There should be a clear pathway for risk assessment (at the booking visit and at every consultation), early identification and treatment. There also should be provision of a multi-professional team meeting on a regular basis.
-
Dedicated specialist service and support:
For conditions such as PTSD / birth trauma, fear of pregnancy and child birth (‘tocophobia’), bereavement and support for mums and dads whose babies are admitted to NICU.
-
Pre-pregnancy advice service:
It is important to have specialist advice and support for women (with PMH illness/ traumatic experience in previous pregnancy) who are considering pregnancy.
-
Patient involvement : ‘Patients first and foremost’
PMH is an area where patients’ opinion must be considered in developing local care pathways. Services must be evaluated on a regular basis based on patient experience.
I firmly believe that all the health conditions should be treated in the same way with professional expertise and kindness and without any prejudice. I am not sure why we still classify health conditions into ‘physical’ and ‘mental’ when there is often an overlap.
Psychological care in pregnancy, delivery and beyond…
It is unfortunate that psychological care has remained a very neglected part within Maternity Services. The reason given for this is ‘the staff are too busy’.
However pregnancy is probably a period of life where psychological support from the HCPs is needed the most.
It is especially important when mums could potentially have severe stress during pregnancy and the postpartum period due to the following factors:
-
Previous history of miscarriage, ectopic pregnancy, IVF, traumatic childbirth.
-
Any other family member or friend has had complicated childbirth experience.
-
Sudden life event such as breakdown in family relation/divorce, loss of employment, bereavement in the family or loved one, relocation/migration and domestic violence.
-
Sexual abuse in childhood or pregnancy as a result of sexual violence.
-
Associated pregnancy complications (for example premature rupture of membrane, high blood pressure, diabetes, concerns on baby’s growth or SPD).
PMH is not only PND and Puerperal Psychosis (PP)…
Many believe that PMH is a term equivalent to the care of Postnatal Depression (PND) and PP.
PMH includes specialised care for women (during pregnancy and one year after the childbirth) with any mental health condition (such as anxiety, depression, bipolar illness, schizophrenia, OCD, eating disorder, and personality disorders).
PMH must include bereavement care (miscarriage, still birth and neonatal death), traumatic birth experience/PTSD, support services for mums and dads whose babies are admitted to NICU and tocophobia (fear of pregnancy and childbirth).
Another important component should be the psychological care of mums and dads throughout the journey of pregnancy, delivery and postpartum period.
PMH, in my view, must be recognised as a separate subspecialty in the training of Obstetricians and Midwives.
Why is identification in pregnancy and immediate postpartum period so important?
-
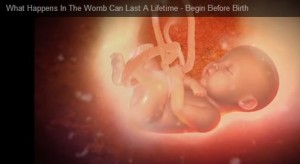
Effects of psychological stress in pregnancy:
There are now plenty of research results, which indicate the long-term impact of stress during pregnancy on the brain development of the baby while it is in mum’s womb. Prof Vivette Glover, an eminent Professor of Perinatal Psychology from Imperial College London, explains this: http://www.beginbeforebirth.org/for-schools/films#womb
Therefore timely intervention and adequate support during pregnancy can prevent long-term effects on the child.
-
Care Planning to prevent serious illness:
All pregnant women with risk factors to develop worsening mental health conditions should have a plan of care during delivery and postpartum period.
Confidential Enquiries into Maternal Deaths have repeatedly pointed out that in the majority of cases of deaths from suicide, there is a lack of care planning during pregnancy.
This is only possible through appropriate care within the Maternity Services and multiagency communication.
-
Enjoying the journey of pregnancy:
Experience of pregnancy and birth creates a lasting memory for the mums and dads for the years to come. Therefore this should be an enjoyable experience for the woman and her family to cherish in happiness in the future.
As HCPs our role is to ensure we support and empower women to make informed choices for the safety of her and the baby and most important of all a very positive birth experience.
-
Helping mums to make informed decision regarding medications:
Mums should get proper advice regarding the use of medication in pregnancy and after delivery.
Pregnancy is a short window but an excellent opportunity to address health conditions.
-
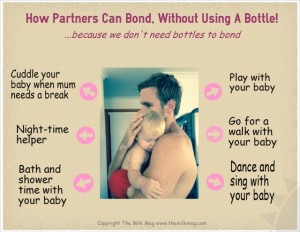
Bonding and attachment:
PMH conditions can adversely affect the bonding with the baby and the mum.
‘A stitch in time saves nine’: Prevention of serious PMH illnesses is only possible through good care in Maternity Services.
Having discussed the importance of the role of Maternity Services in PMH, now let us find out what is happening in the Maternity Units……
A journey of revelations…
I contacted many Maternity Units across the country to find out the provision of PMH services within their Units. What I found was extraordinary.
I raised my concerns in a letter published in The Guardian: http://www.theguardian.com/society/2015/oct/14/perinatal-mental-health-provision-badly-lacking .
I raised this issue with the Maternity Review Team, during my meeting in September (2015).
Although there are examples of good service, the overall structure within the Maternity Units is very poor:
-
Often there is no dedicated Lead Obstetrician and/or Specialist PMH midwife
-
Many Units do not have formal debriefing services (for traumatic birth experience), specialist bereavement midwives and support system for parents with babies admitted to NICU.
-
There are hardly any dedicated services for women with fear of childbirth.
Delving deep into the challenges….
To have a better understanding of the need, I embarked on a journey to meet professionals from all the relevant Royal Colleges (RCOG, RCM, RCPsych, RCGP), Health Visitor organisations, Maternal Mental Health Alliance (MMHA), MPs and All Party Parliamentary Group (APPG), NHS England, CCGs and other national Campaign Groups.
It was revealed that overall there is very little understanding of the vital role of the Maternity Services in PMH.
Thankfully RCM is campaigning for a Specialist Midwife in every Maternity Unit.
But the main barriers are the following:
-
Lack of Mapping of the existing services in PMH within Maternity Units (such as the MMHA map of the available Perinatal Psychiatry services).
-
Lack of a national standard of the service provision within Maternity Units (according to the number of deliveries and complexity of cases).
-
Poor collaborative work among HCPs: as often the Maternity Electronic record system is not accessible to other HCPs and vice versa.
-
Lack of standard Training programme for the Obstetricians and the Midwives.
-
Lack of adequate focus on PMH illnesses in Antenatal Education.
I have concerns that unless these issues are resolved appropriately, we cannot provide the best quality of care for women with PMH illnesses.
With the best of my abilities, I am currently working closely with other national organisations to address these areas.
Maternity HCPs: Please, please do something and don’t wait for things to happen….
It is true that funding is necessary to set up specialised PMH services and Mother and Baby Units (MBU). However Maternity Units should not wait for the approval of their business cases.
In my humble opinion, funding is not everything. Our professional values are the most important factors in patient care:
-
Kindness:
Simple measures such as a smile, empathy and a willingness to listen to the concerns of the mums and dads could make a huge difference in patient experience.
-
Communication:
Take every opportunity to explain the situation and ensure that appropriate wording is used during communication.
-
Continuity of care:
Try to ensure continuity whenever possible or communicate adequately with the rest of your team.
-
Local Alliance:
Please try to develop Local Alliances with Community Midwives, Health Visitors, GPs, all available community mental health services, Peer Support groups and children’s services.
This could significantly improve communication among the multi-agency teams in caring for mums with PMH illnesses.
-
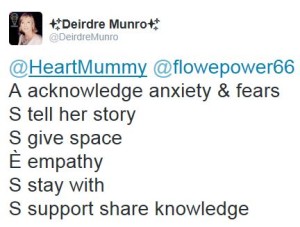
Listen to concerns:
Please create opportunities to listen to the concerns of the user group. This may be in the form of promoting your local Maternity Service Liaison Committee (MSLC) or Patient Panels.
If possible, please read the real life stories of the Lived Experiences on the Internet: it would help you to think ‘outside the box’, have a better insight into the PMH illnesses and give you inspiration.
-
Raise awareness:
Arrange patient engagement events, Road shows or Community Events with local CCGs.
Participate in Social Media support, such as #PNDHour (Wednesday 8-9pm) and #BirthTraumaChat (Monday 8-9pm):
This would help to raise awareness, remove stigma and give mums and dads a ray of hope.
-
Arrange training on PMH:
Please ensure all staff are adequately trained in your local Units.
-
Get involved in your Regional PMH network:
Many regions now have regional PMH Networks. This could be an important place for information sharing among the Maternity Units.
-
Please do not forget dads:
There is now good evidence to support that dads can suffer from PTSD/PND. Please take every opportunity to support and communicate with dads.
-
Keep yourself updated:
PMH is a rapidly evolving area; therefore HCPs must keep their knowledge and skills up-to-date through continuous professional development.
If unsure, please seek help and escalate to your senior colleagues: an unsafe advice from a HCP could endanger an invaluable life.
Working together to make a difference…
We ALL need to work together to prevent suffering and death from PMH illnesses.
If you have any suggestions for improving PMH services within Maternity Units, I would be very keen to know (Twitter: @RajaGangopadhyay3).
If you are involved in good projects locally or are aware of any good practice, please share with everyone through #MatExp.
Acknowledgement
I am grateful to #MatExp for giving me this opportunity to write this blog.
I am immensely grateful to all the Lived Experiences for sharing their stories, which have enriched my knowledge on PMH much more than any textbook and journal article.
My thoughts are with all the bereaved families who have lost their loved ones due to this dreadful illness.
Raja Gangopadhyay
2015


























 via http://www.pantley.com/elizabeth/%5B/caption%5D
via http://www.pantley.com/elizabeth/%5B/caption%5D