When people think about post traumatic stress they often think of a soldier, returning from battle traumatised and battered by the ravages of war and the terrible things seen and experienced.
However PTSD doesn’t only affect those affected in the aftermath of war or a terrible natural disaster or violent act. PTSD can also affect someone in circumstances that should be safe, that should be happy, that should be the start of an amazing journey. For some women the birth of their baby can be traumatic and can be a trigger for PTSD that can severely affect their life. It can affect bonding with their baby, relationships with family and friends, doing everyday activities and physical health. So what is birth trauma and PTSD and how can we help and support women that are suffering?
Firstly what is birth trauma?
‘Birth trauma is in the eye of the beholder’ (Cheryl Beck) and this is true. What is traumatic to one woman may not be traumatic to another woman. Each woman’s experience of birth is unique to her and many things can add to a woman feeling her birth was traumatic. For some it maybe that her birth was a truly scary event, she may had been in an emergency situation where her life and that of her baby was at risk. Maybe her labour was very lengthy and very painful. It may be that a woman’s birth had high levels of medical intervention, such as induction, caesarean section, episiotomy, or other medical issues. It may be that a woman gives birth early and her pre-term baby requires care in NICU. Sadly some women have a birth that results in damage or injury to her baby and some lose their babies at birth.
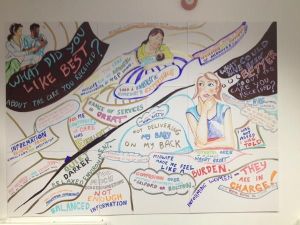
For other women trauma can result from the way she is looked after by the staff responsible for her care both during the birth of her baby but also postnatally. She may feel a loss of control, dignity and privacy. There may have been a lack of information or a woman may feel she wasn’t listened to and her choices not respected or overlooked. She may feel she had medical procedures done without her consent or without proper explanation or that she was left with no choice. Or maybe unkind, cruel words and actions made her feel vulnerable and exposed.
Some women find birth triggers or adds to previous trauma such as rape or domestic abuse.
Often women who feel traumatised from their birth will feel isolated, other women may not understand why she feels traumatised, after all isn’t childbirth a ‘natural thing’? So a woman can feel guilty and somehow ‘weaker’ than other women for being unable to ‘cope’ with birth . She may feel she should be over the ‘birth’ and often well meaning friends and family will say things such as “at least you are ok and you have a healthy baby”. This only confounds the woman’s feelings and makes her feel more isolated and can damage relationships with partners, family members and friends as a woman feels no one understands and so she withdraws deeper into the trauma. Depending on the nature of the trauma a woman may feel unable to have further medical tests such as smear tests. Sex may also be affected as a woman may fear further pregnancies, or even just the act of physical intimacy itself. Many women who suffer birth trauma may struggle to bond with their baby, others become overly anxious of their babies health and wellbeing and constantly worry about every aspect of caring for their newborn.
For a woman that has lost a baby during birth or whose baby has been injured during birth she may experience overwhelming guilt, she may feel like it is her fault that she somehow failed her baby or that she should somehow have prevented it. She may play over and over again the birth in her head seeking answers or ways she could have changed the outcome.
Feeling like they have no voice, are misunderstood and weak many women will seek to hide their true suffering and ‘carry on’, the weight of trauma bearing down on them crushing hope, light and happiness as they try desperately to cling to normality. Everyday tasks become hard and just coping day to day can feel overwhelming. Their physical health too may suffer, as the effects of trauma ravage them mentally. Lack of sleep, trouble eating and the constant struggle all takes its toll. Flashbacks may take them back to the event reliving moments, even smells and conversations causing great distress and anxiety.
So what is PTSD and how does it differ from postnatal depression?
Often women can be wrongly diagnosed with PND when in reality they have PTSD. While PTSD and PND can overlap as they do have some similar symptoms, they are very different. Its important that a woman receives a correct diagnose so she can have the support, help and therapies she needs. PTSD is the clinical term for a set of normal reactions to a traumatic, scary or bad experience or event. It can occur after a person experiences or witnesses something that was or they perceive to have been life-threatening.
Signs of PTSD include:
- Feelings of intense fear, helplessness and/or terror.
- The re-experiencing of the event by recurrent intrusive memories, flashbacks and/or nightmares. The individual will usually feel distressed, anxious or panicky when exposed to anything which remind them of the event.
- Avoidance of anything that reminds them of the trauma. This can include talking about it, the place where the trauma happened or people that may have been involved in the trauma. (such as hospitals, doctors, healthcare professionals) Even T.V programs or books maybe avoided.
- Bad memories and flash backs often result in difficulties with sleeping and concentrating, thus affecting daily activities. Sufferers may also feel angry, irritable and be hyper-vigilant or jumpy, easily startled.
- Suffers may suffer panic attacks, depression and anxiety. They may feel detached, alone and have a sense of something bad may happen to them or their loved ones.
It is important to remember that PTSD is beyond the sufferer’s control. It is the mind’s way of trying to make sense of an extremely scary traumatic experience and are not a sign of an individuals ‘weakness’ or inability to cope. The person cannot just ‘get over it’ or ‘pull themselves together’ or ‘move on’. Rather they need help and support to process not only what has happened to them but also the feelings surrounding it.
So what can help a woman who has suffered birth trauma or PTSD?
For partners, family and friends its important to acknowledge what has happened to the women and her feelings surrounding it. Encourage her to talk about her feelings if she is able to. Help her to see you want to try to understand how she is feeling and that you recognise how traumatised she may feel. Reassure her that you are there for her and that you will help in anyway you can. You maybe the only person that she trusts. Encourage, commend show compassion and empathy. Emotional support is invaluable, even if it’s just a listening ear or a hug. Realise that there may be things or activities that she may not yet feel ready to do, be patient and show understanding.
Encourage her to get help, whether it be her GP, health visitor, midwife or a charity such as the Birth Trauma association or Mind. This will not be easy as she may have a fear and distrust of telling anyone how she really feels especially a healthcare professional. Reassure her of your support, maybe offering to attend any appointments with her if she wishes. Asking for help will be hard, and so will the time undergoing any therapies being there for her providing emotional support is so important.
Also, helping with daily activities can mean so much, helping her get much needed rest offering to prepare a meal, or to do some shopping can also be invaluable.
Helping someone with PTSD can be difficult and frustrating.Partners and family can feel lost and confused too. Reading up on PTSD can help you understand it and how it can affect someone that is suffering.
Of course some partners too can feel traumatised and suffer from PTSD after seeing the birth of their baby. It is important they too seek help and support.
What about healthcare professionals?
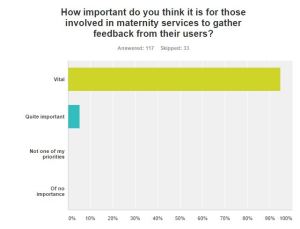
Its important that any healthcare professional’s when supporting a woman after birth build a relationship built on trust. LISTEN, this is the single most important thing to a woman who is suffering. Listening enables you to truly know what she has been through, how she is feeling and whats important to her and her family. Listening will enable you to know if she is likely to be suffering PTSD or any other perinatal mental health disorder. Listen also to her partner and family, they know her best, if they feel something isn’t right or reach out for your support then be there. Ask for training in order to help you understand the different types of perinatal mental health issues and know the pathways and any local support available to signpost a women to. Be careful of language used and do not minimise her feelings or experience. If you know a woman has had a traumatic birth from postnatal notes etc, ASK, don’t ignore it.
What can a woman who has had birth trauma/PTSD do for herself?
- Speak to someone, partner, family, friends, midwife, health visitor, GP. Don’t suffer in silence.
- Remember you are not alone, there are others too that have been affected by birth trauma.
- Remember you are not to blame.
- Look after yourself, make sure you rest and eat a good balanced diet. Do things, activities that help you to relax.
- Know your limitations and what you can do both physically and emotionally.
- Speak to your hospital about your experience. Some women ask to see their medical notes and discuss exactly what happened to them and why.
- Seek help and treatment. There are various treatments for PTSD such as counselling, Eye Movement Desensitization and Reprocessing (EMDR), cognitive behavioural therapy (CBT) and medication.
- Find local support groups or support groups on social media (such as birth trauma facebook support page)
Birth trauma is real and so is PTSD, its important that women get the help and support they need to overcome it. The birth of her baby can affect a woman for the rest of her life, it may not be possible to completely prevent birth trauma but what we can do is support women when things do go wrong and make sure that we show them love, compassion, kindness and help even at the darkest times so they believe that it will be possible to bathe in light again.
Emma Jane Sasaru