Originally posted September 26, 2016 by Leigh Kendall

This post was written by Leigh Kendall, mum to Hugo who sadly died aged 35 days. The post was originally published on 26 September, 2016 on Leigh’s now defunct personal blog. You can get in touch with Leigh on Twitter at @LeighAKendall.
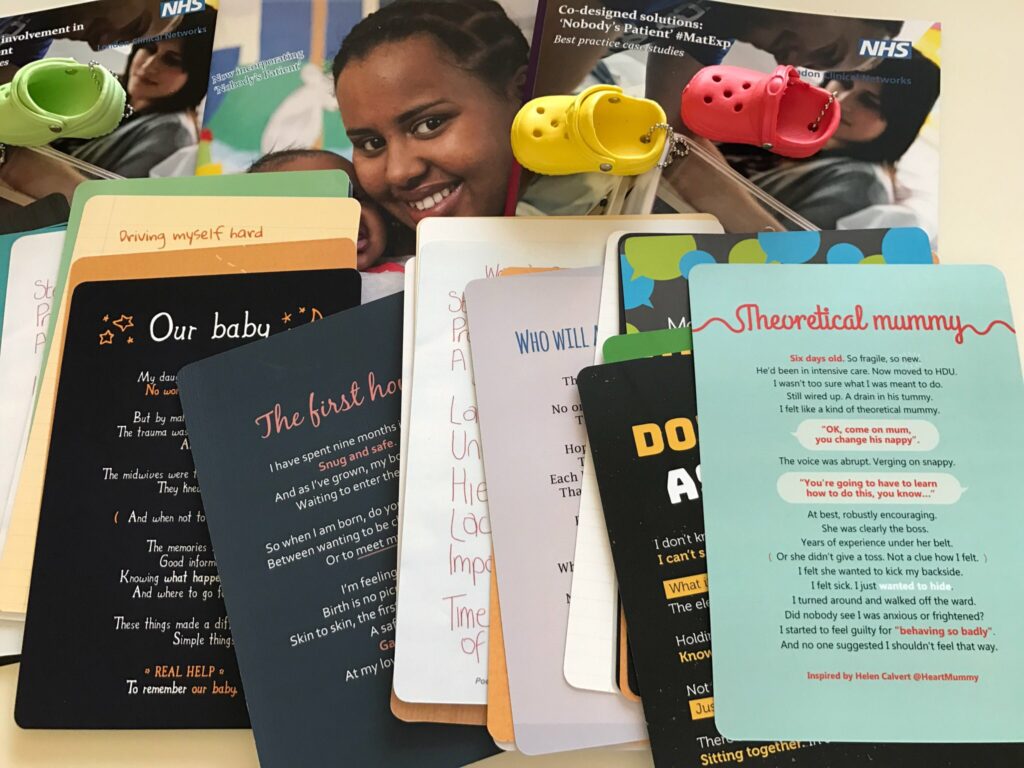
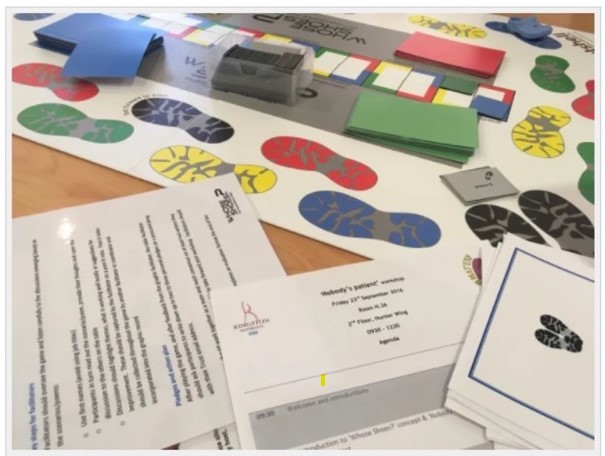
Nobody’s Patient workshop: St George’s Hospital – 26 Sep 2016
Friday September 23 was a special day, one I have been waiting on for a long time: the Nobody’s Patient workshop at St George’s Hospital.
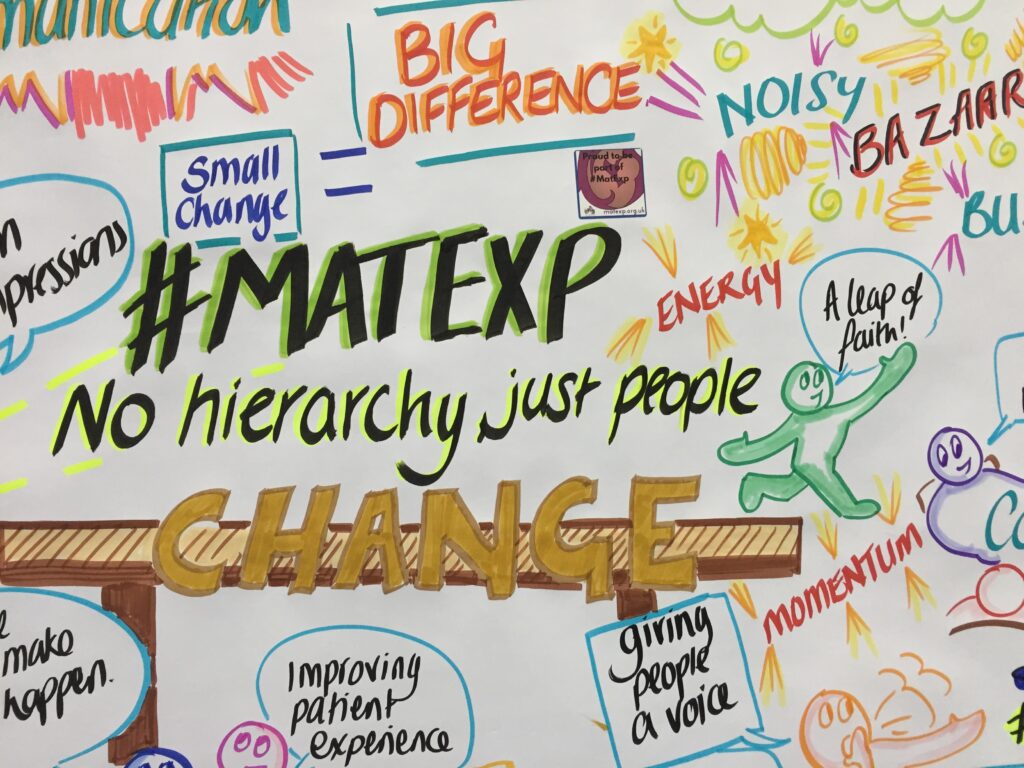
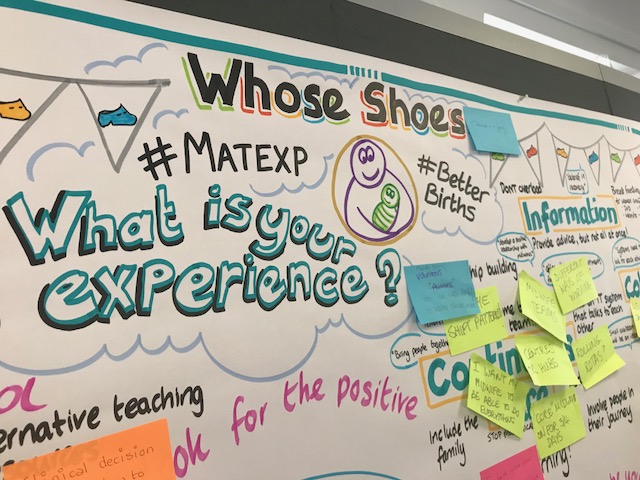
The workshop is a key part of the Nobody’s Patient project and received funding from the Maternity Review Challenge Fund . The project evolved from the grassroots social media change platform #MatExp, and was inspired in part by my experiences with Hugo.

Bringing Nobody’s Patient to St George’s, where Hugo was born, lived and died is an achievement that means so much to me that it is hard to fully express using mere words.
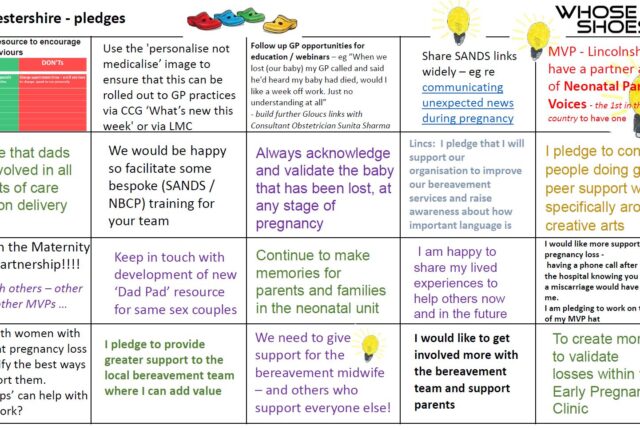
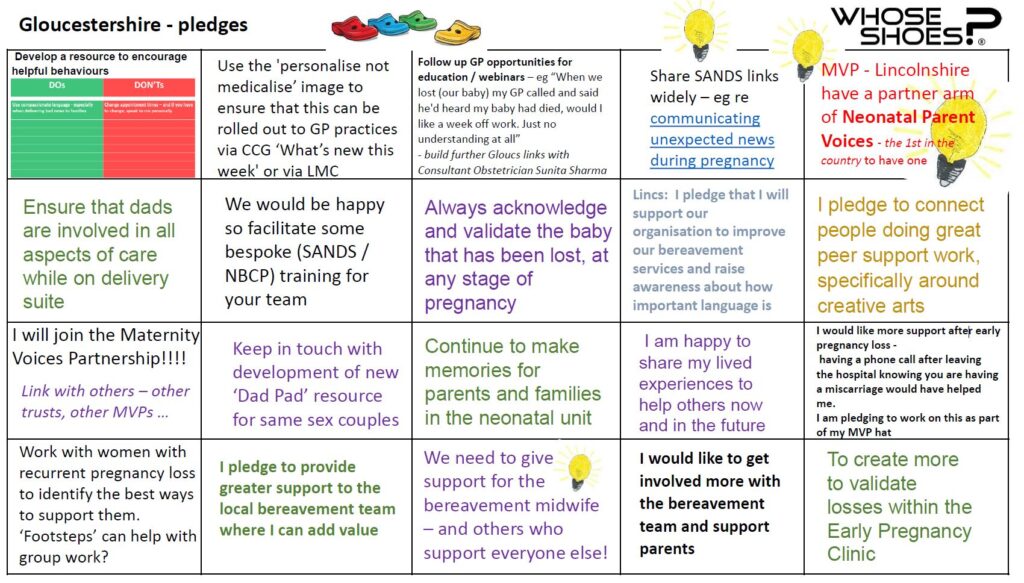
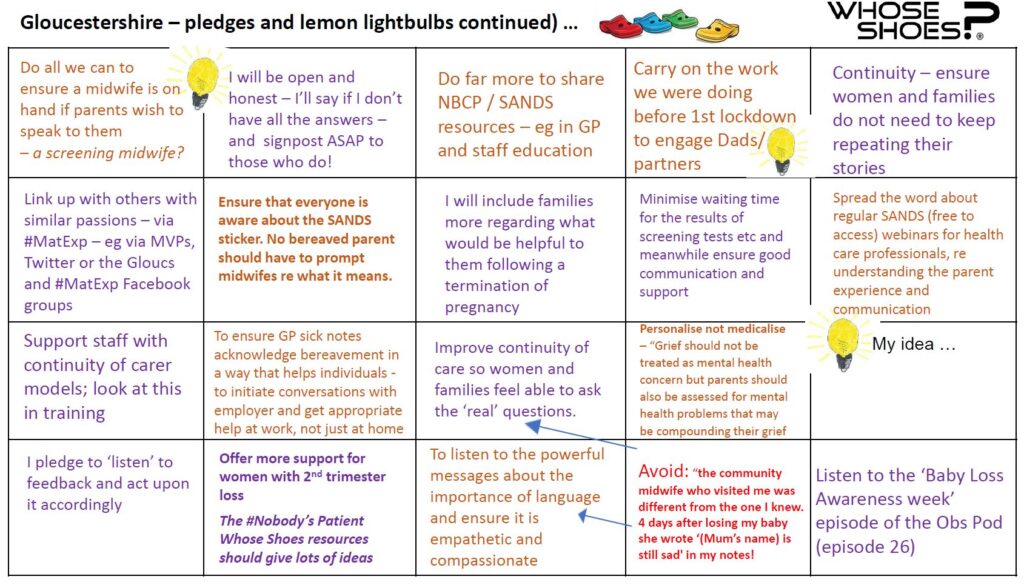
The aim of the workshop was to get health care professionals involved in caring for families like mine to understand more about our experiences, and to make pledges to improve experiences for other families. I can’t change what happened to us, but through #HugosLegacy I wanted to help future families’ difficult experiences be a tiny bit easier.
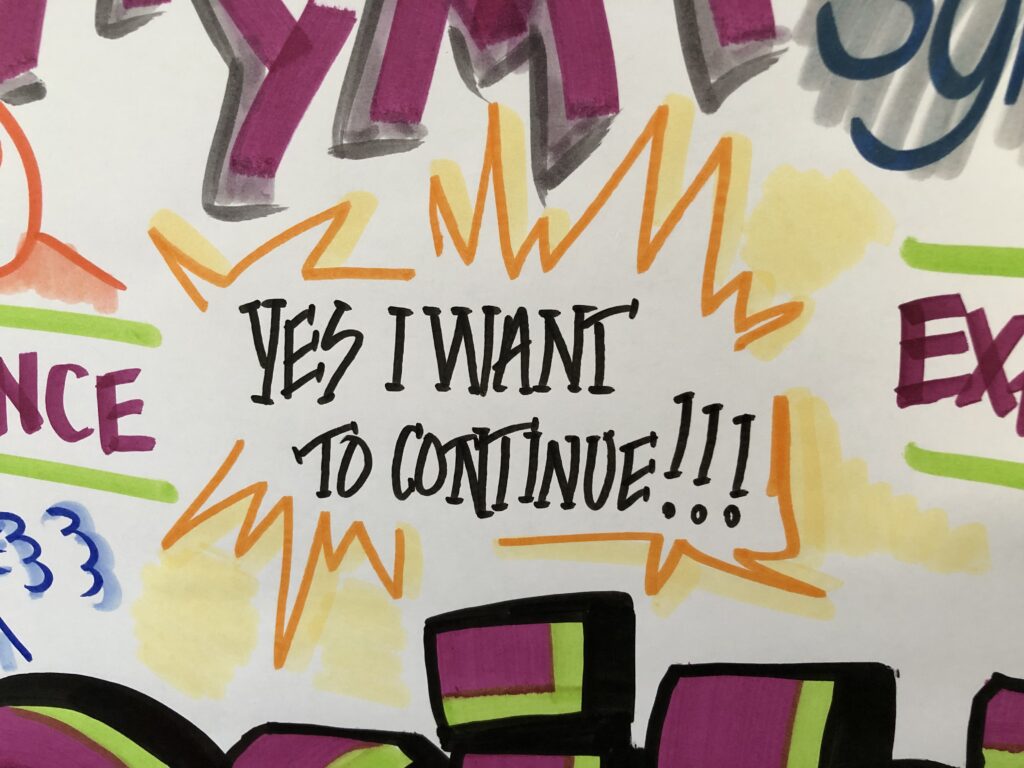
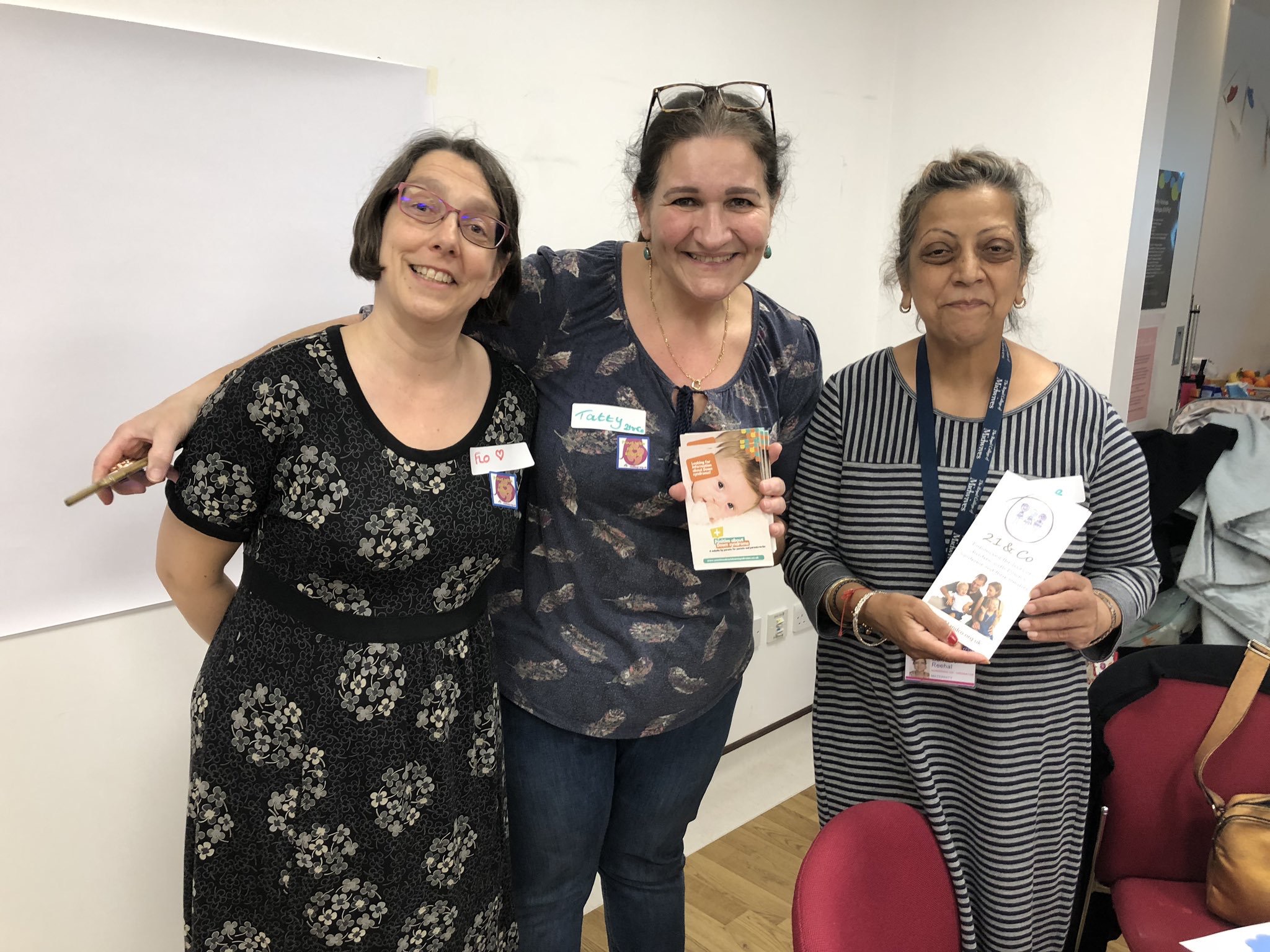
The first workshop, in Kingston in early July 2016 was a huge success – everything was crossed for St George’s to emulate that. I was delighted to see so many people attending the workshop – all busy people prioritising the workshop over the million other things they have to do.

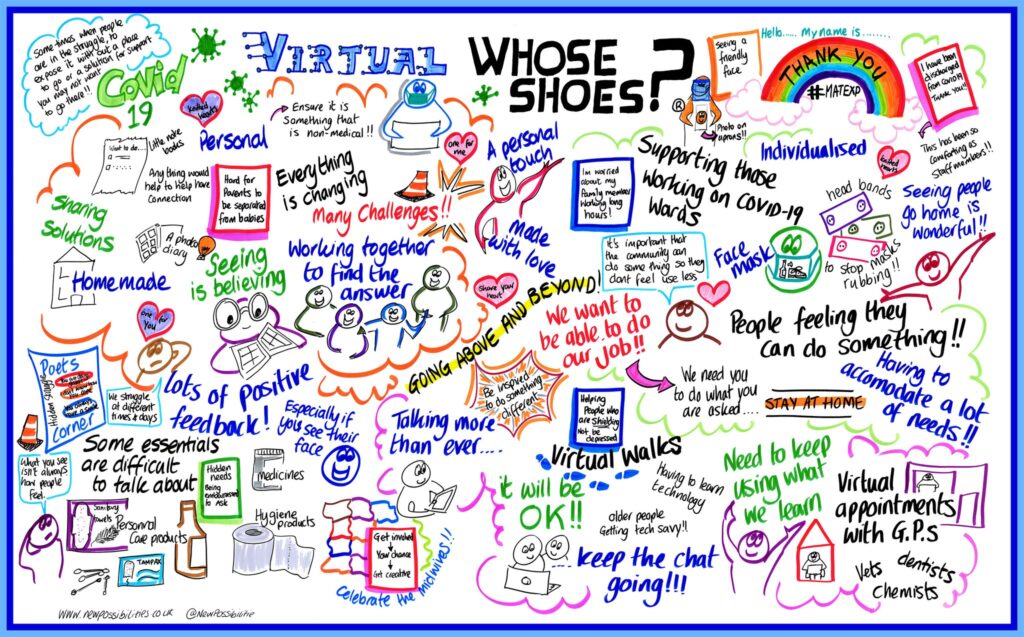
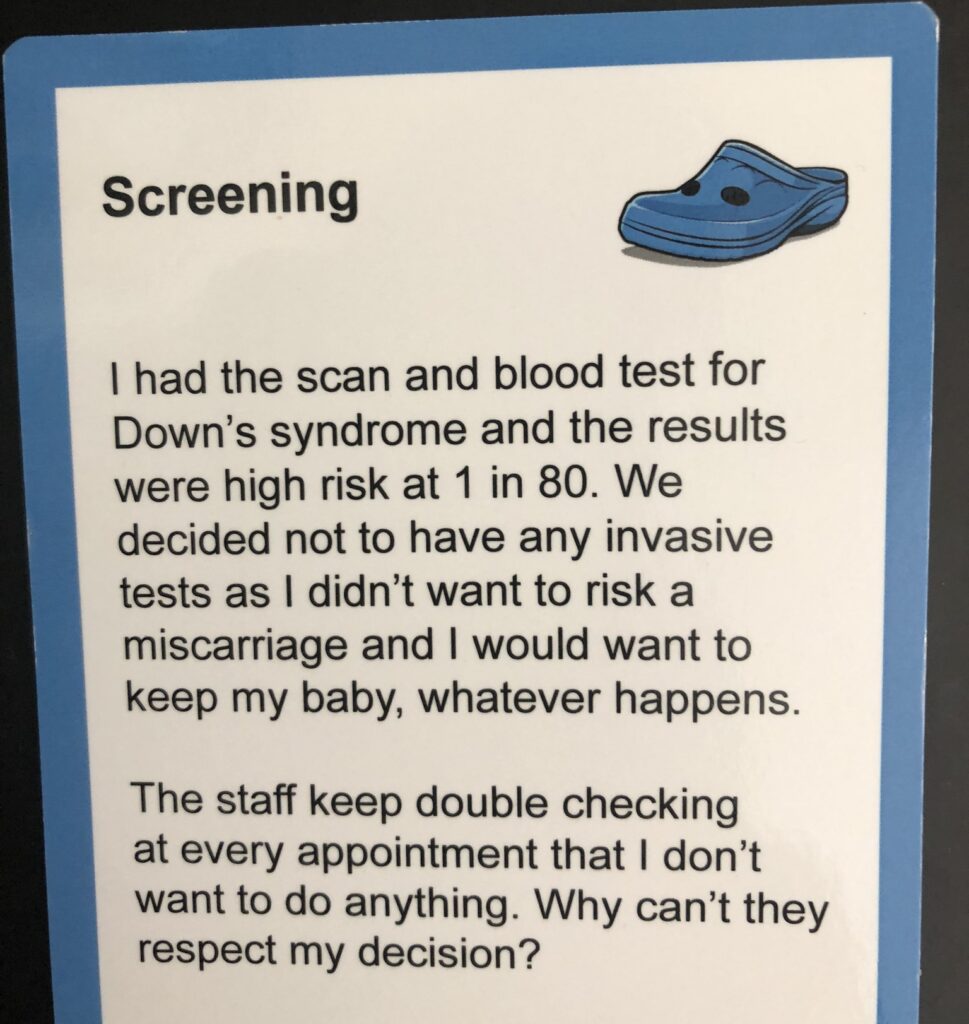
The workshop got underway: the room was full of buzz and ideas. Participants barely even stopped for refreshments so engrossed were they in the scenarios and discussion. All the scenarios are sourced from real people’s real experiences, which makes them very resonant, relevant, and often emotional – for both negative and positive reasons.
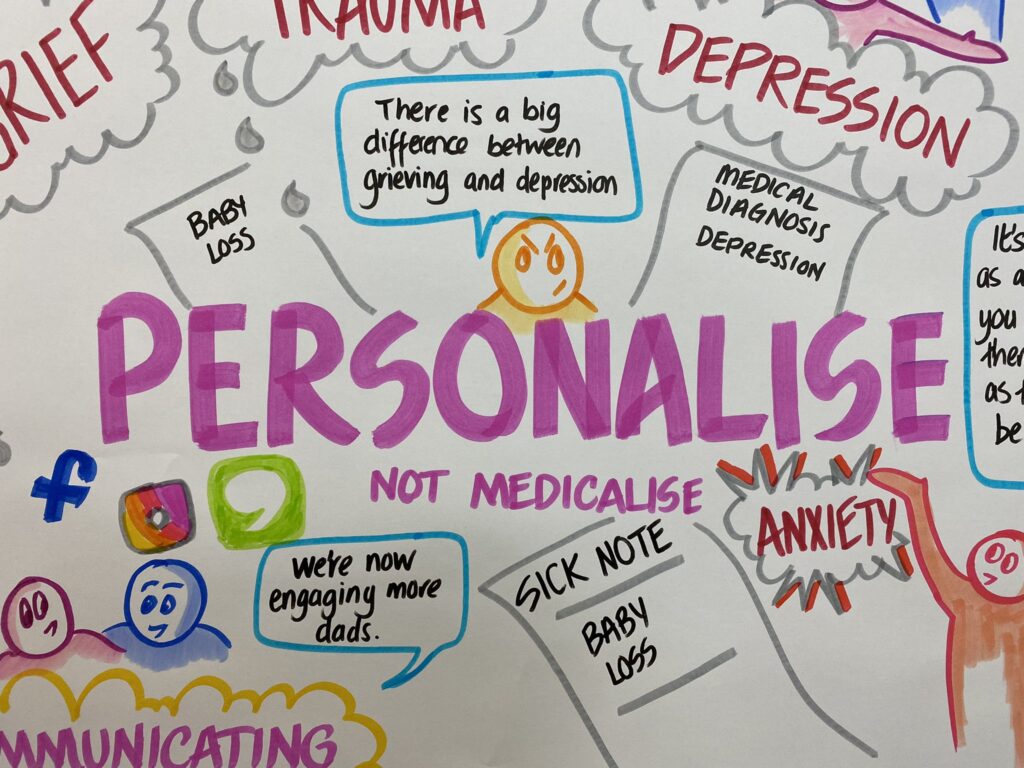
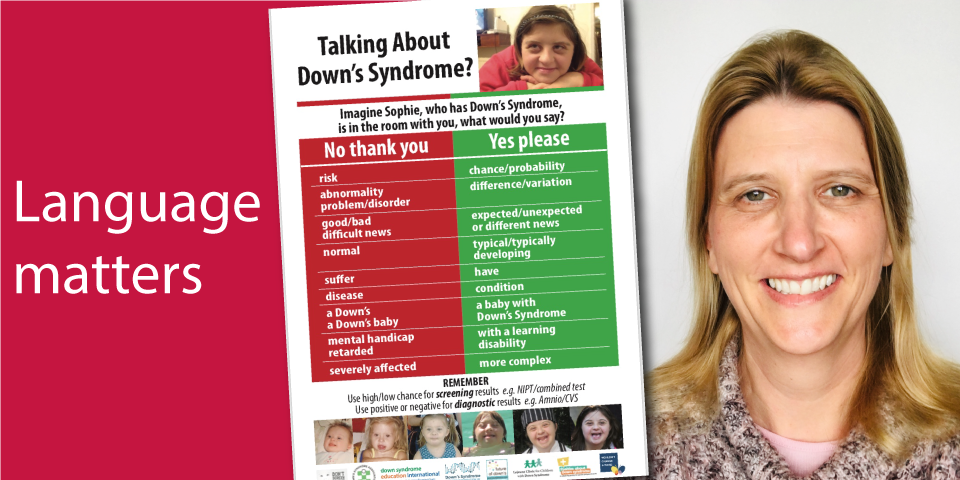
Communication was of course a topic that underpinned many of the discussions. Some of the key points from the table I was on include:
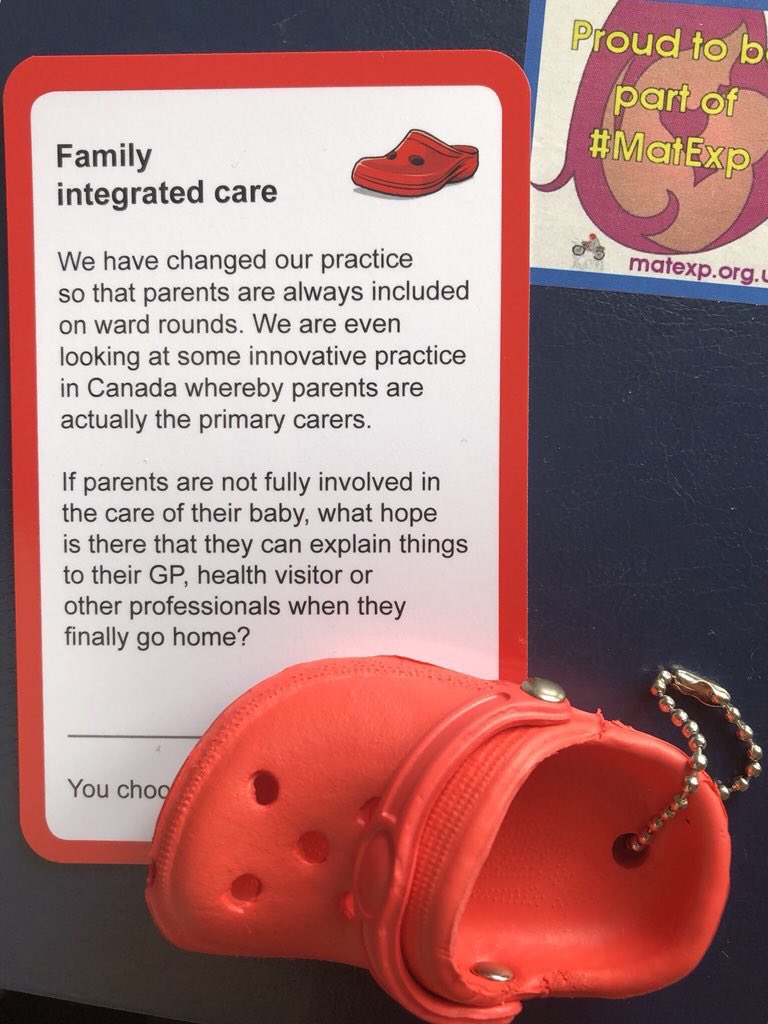
- The suggestion that doctors could use drawings to help parents understand their baby’s condition. Parents are tired, stressed, and emotional – being in the NNU can feel like you need to gain a medical degree within days, and there is so much terminology to learn. Parents are constantly anxious, and their precious baby being attached to an array of beeping machines that are keeping their baby alive adds another level of terror. Visual aids such as drawings of anatomy can help parents understand – and in turn these drawings can help parents explain their baby’s condition and prognosis to family and friends, too. Doctors shouldn’t worry about their art skills – it’s about the concept rather than it being perfect! Anything that helps parents grasp complicated concepts is positive. There are some worries about notes and the formal medical record and governance, but the consensus was that drawings used as part of a conversation with parents are separate to the formal medical notes.
- NNU mums often have difficulties receiving the necessary postnatal checks (whether or not they were ill during pregnancy, as I was). NNU mums’ priority is their baby, but their health matters too: they need to be as healthy as possible so they can be there for their baby, whatever the outcome. Our table discussed the concept of a ‘virtual ward’ where NNU mums could have their postnatal checks by identified professionals who crucially would have some training in the needs of NNU mums. Emotional and psychological needs of NNU parents are very often missed.
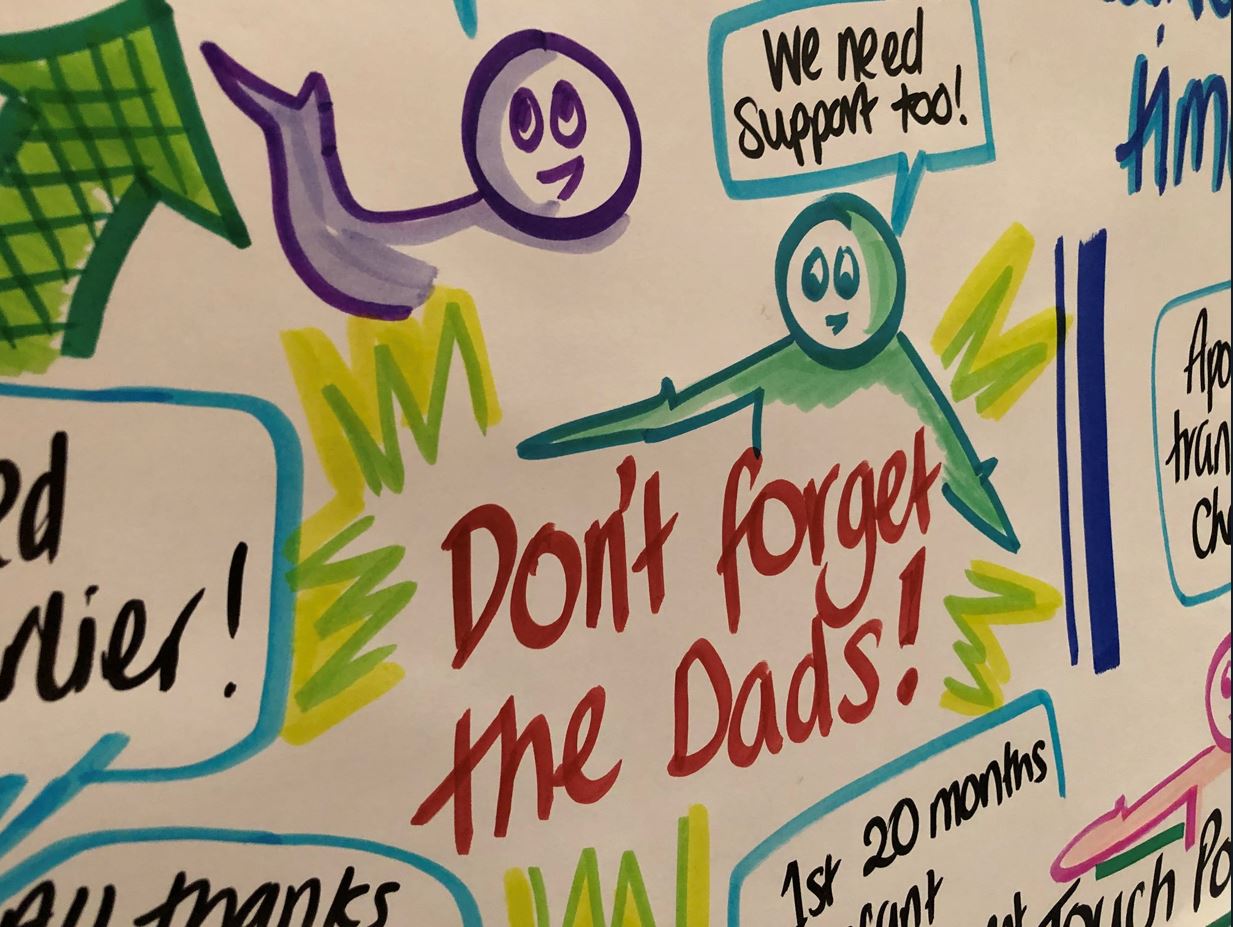
- Dads and partners matter! Our table discussed how dads can be left out of the equation. There are times where they have been left alone after a traumatic birth, with blood everywhere and the in the delivery room looking like a scene from a horror film, their wife/partner and baby having been whisked away. The group talked about how in an emergency situation the room will be full of a range of professionals doing what needs to be done. Even if the procedure or equipment is routine, it may seem terrifying to the relative. Often after the emergency all the staff will leave the room with the patient, or go off to attend to other matters. Someone needs to remember to speak to the relative, debrief them, keep them updated, and give them information – not leave them standing panic-stricken.
- I was heartened, especially after the disjointed nature of my own care, to see the dedication of professionals from various specialties keen to work together to give these mums and families the best possible experience and minimise additional stress.
In case you don’t have time to watch the whole video, some highlights amongst the many excellent pieces of feedback and pledges are:
- A method of parents keeping an eye on their baby even when not physically present, eg FaceTime. This would have been so helpful to me when I was in intensive care in the hours before I was able to go and see Hugo, and for both Martin and I when we had to go and rest. Every neonatal parent needs to rest, and some parents need to go to work and/or care for other children too, so making use of technology would help parents feel able to be close to their baby at all times.
- To see the mother and baby as one unit. The postnatal ward and NNU currently do not communicate well with each other; these links need to improve. In particular, the postnatal ward needs to better recognise the needs of NNU mums with things like expressing breast milk; food, emotional support, and being in the NNU with her baby as much as is possible.
- Ideas to help parents understand and get involved with their baby’s care as much as possible, for example emoticons on the incubator to signify how the baby is doing.
- The need for kindness, empathy, and understanding for any parent who is seriously ill during pregnancy, whose baby is cared for in an NNU, or whose baby dies at any stage during pregnancy.

After the conclusion of the workshop, we spent a lovely couple of hours in the First Touch garden, soaking up the glorious sunshine. This garden was designed by a NNU dad (whose lovely wife is also the charity’s director) and won a prize at Chelsea. The garden was moved to the front of the hospital for everyone to enjoy.

I would like to say a heartfelt THANK YOU to everyone who made this workshop a reality through organising it, and to everyone who attended. Martin and I cannot change what happened with me, and we cannot bring Hugo back. Helping other families through Hugo’s legacy helps us by knowing that Hugo can never be forgotten, and that his life has had purpose.
St George’s has been brilliant at listening to the feedback I have given them about the experiences of my own care and Hugo’s care, and has already implemented many improvements where necessary. I shall always be grateful to the hospital for saving my life, and for giving us 35 precious days with Hugo. The hospital and the staff who work there will always have a special place in my heart.
And, of course, Nobody’s Patient is about more than me, Martin, and Hugo. It is about ALL families who find themselves in a similar situation. We are working together to help prevent other families falling between the cracks of services, and avoid unnecessary additional stress and upset.
The St George’s and Kingston workshops are part of a pilot that we hope other hospitals nationally will take on board.
Because nobody should feel like they are nobody’s patient.