There have been some fantastic conversations taking place on the MatExp Facebook group, with a new ACTION thread every day to generate discussion. The aim of these discussions is to identify ways that we can ACT to improve maternity experiences. Big, long-term actions that might require system change or a change in culture. And small, immediate actions, that professionals and individuals can take today to improve the maternity experience of those around them.
One of the first topics we looked at was Anxiety, as it had been one of the first issues raised on the MatExp ABC.
“Anxiety” covers a number of areas when we look at maternity experience. Mothers can have existing problems with anxiety, that have already been identified. They could have had anxiety for some time but the experience of having a baby has intensified it (my experience). It could be that they begin to suffer with anxiety postnatally – Emma Jane Sasaru has written here of her experience of perinatal anxiety. Or perhaps their anxiety is focused on giving birth – many mothers are incredibly anxious about what the end of pregnancy has in store for them. Finally, there will be mothers who have experienced birth trauma or baby loss and this can understandably provide a background for anxiety in subsequent pregnancies.
Anxiety UK says of anxiety that it is “something that can persist whether or not the cause is clear to the sufferer”. The organisation lists the symptoms as
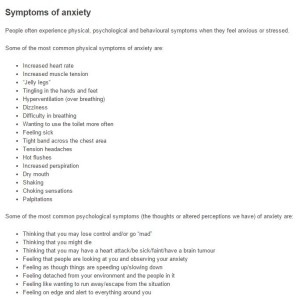
Certainly, on a personal note, “feeling detached from your environment and the people in it” goes some way to explaining why it took me such a long time to properly “fall in love” with my babies. There was no “rush of love” for me when I gave birth and first held my children, despite my having positive birth experiences both times. “Feeling like wanting to run away / escape from the situation” – many new mums feel like this at times when coping with a newborn baby but it is important to recognise when feeling like this “now and again” has accumulated into something more problematic.
So how can we ACT when anxiety is a factor in maternity experience? Let us first look at how women can help themselves:
- Practice HYPNOBIRTHING – a number of people involved in the #MatExp campaign suggested this as a great way to alleviate anxiety in pregnancy and anxiety about birth itself. Pregnancy Coach Suzy Ashworth explains here what hypnobirthing is all about, and how it’s beneficial for all women regardless of the way they plan to give birth.
- BE HONEST and try to explain your anxieties to your healthcare professionals. Find out as much as you can about anxiety and ways to manage it.
- GET HELP.
Now these actions all assume that the woman in question is aware that she is struggling with anxiety. But this is certainly not always the case. This is where the birth professionals come in. How can they act when anxiety is a factor?
- Understand how anxiety can manifest itself. If a women is finding it difficult to talk about something, if she is quiet and refusing to engage with a situation, if she practices avoidance by walking out on a conversation then think “anxiety”.
- Give women the opportunity to talk openly about their fears, and really LISTEN.
- Offering reassurance can be helpful but it can also be dismissive – being told “don’t worry, that won’t happen” can heighten a woman’s anxiety as she will feel as though her fears are not being taken seriously. Always remember that those fears are REAL to her, however bizarre they may seem to you
What services are available to women in your area who are struggling with anxiety? Are the following available (and do you know how to access them?) or do they need to be put in place?
- Hypnobirthing, mindfulness and meditation classes
- Cognitive Behavioural Therapy (CBT)
- Specialist mental health midwifery teams
- Training for midwives and health visitors on recognising anxiety
Where services are available, there are simple ways in which women’s access to them could be improved:
- Please check on the mental health of the women you care for throughout their pregnancy and postnatal period, not just at their booking in appointment.
- If you offer anxiety support, please make it possible for women to enquire about these services by email, not just by phone. Phone conversations are very difficult for many anxious people, and services only being accessible by initial phone assessment put up a real barrier.
When we look specifically at prenatal anxiety, there are changes to our birth culture that could make a big difference:
- Empower women to trust their bodies. Too many women fear that they will not be able to give birth safely – how can we help them to understand how their body works and reacts in labour, and how it can be supported and encouraged to do its job?
- Ensure that women understand that they have the control to make their own birth choices. Feeling as though they have no control is a huge factor for anxious people, but encouraging informed choice and putting women at the centre of their birth experience can help to alleviate this.
As with almost every discussion of maternity experience, continuity of care becomes an issue. Where women know their birth professionals and have built up a relationship with them, anxieties are reduced. Whilst continuity of carer is offered in places on the NHS this is far from the norm at this moment in time. If you struggle with anxiety then there are care options available to you to ensure that you have continuity in pregnancy and beyond:
- Use an independent midwife. There is a cost involved in engaging the services of these professionals, but it is always worth speaking to them before dismissing the idea on the basis of cost, as there may be ways that the cost can be reduced.
- Use a OnetoOne midwife. This is a “free at the point of delivery” service, but unfortunately it is only available in some areas. Find out if they are commissioned near you.
- Use a doula. Doulas support women and their families during pregnancy, childbirth and early parenthood. This support is practical and emotional but non-medical in nature. Again, there is a cost involved, but there are ways that this can be reduced so it is worth contacting your nearest doulas to discuss the options open to you.
Lindsey Middlemiss (aka “Newbury Doula”) is having lots of discussions at the moment about the wider provision of doula support for women with high anxiety of at high risk of PND, including women who have experienced baby loss or who have had birth trauma. There is a possibility of some NHS funded pilots and research studies in the future, and the Doula UK Access Fund will likely be changing and expanding its criteria. We eagerly await developments in this regard.
#MatExp “Language” Champion Leigh Kendall has written extensively about support for bereaved parents and I know she will be suggesting further actions during #FlamingJune. Therefore I don’t want to focus too much here on anxiety in those who have experienced loss, but one thing did come out loud and clear from the discussions we had on Facebook:
There is currently no standard care pathway for those who are pregnant following the loss of their baby. They might be labelled “high risk” depending on whether baby loss was a result of pregnancy complications, but their emotional needs are not automatically met.
This is staggering to me.
This has to change.
On a positive note, one member of our community is aware of midwives at her local hospital looking into setting up Rainbow Antenatal Clinics specifically for those who are pregnant following loss. Is this something that you could look into at your hospital? Is this something you already offer?
Another positive that I would like to finish on is the new provision of antenatal appointments from our health visiting teams. Vanessa (aka Frustrated HV) had this to say on the subject, with specific reference to pregnancy following loss:
“I really do hope that the antenatal visiting programme being undertaken by health visitors & the increased communication between midwives & health visitors & GPs will mean that fewer women experience this neglect… Because it has to! A known history of loss in or around pregnancy should now automatically trigger (through midwife reporting) a Universal Plus antenatal health visiting service. Which would mean that you would have support throughout the pregnancy (as well as after) & signposting/referral to more specialist services if needed. No one should still be experiencing this type of trauma. You are correct that lots still needs to be done, but lines of communication are being created & general awareness is improving & I know that with the continued efforts of all the people I have seen in #MatExp & through all the conversations & wisdom shown, we will change things for the better.”
Join the conversation. #MatExp #FlamingJune