A while ago we decided to pick six words that we felt really summarised Matexp. As with the healthcare six C’s, we very much wanted our values to reflect what we feel is important to a good maternity experience both for families and staff. So with this in mind, the six values we chose were;
Choice
Kindness
Language
Respect
Dignity
Compassion
We set about asking everyone on facebook and twitter what each of the values meant to them.
Choice
Our first word was choice and we knew when it comes to maternity experiences is so important to families. So what did everyone say about choice?
“Choice to me means having the same services and facilities available to all women. Birth experiences shouldn’t be a postcode lottery.”
“Choice to me means being presented with the correct information so you can make an informed decision. An informed decision is an empowered one.”
“Choice means to me, that all women whether low risk or high risk have access to the same facilities & are given the opportunity to make an informed decision to choose how & where they birth without judgement or pressure even if it is not medically advised.”
“Choice to me means that we give families accurate, unbiased info so they can make a informed choice that is right for them. Then support them in that choice.
“Listen, really listen to women and let them pour out their heart and get to know what they need to make their birth what is right for them.”
“Choice is about being given all the information you need to make a decision in an unbiased, non-pressurised way.”
“Choice is being told the benefits and risks associated with each option. Choice is being told the benefits and risks with your alternative options (it’s very rare that there is no alternative option).
Choice is being told what happens if you simply do nothing. Choice is knowing how decisions made now will effect your future, I.e.surgery can have implications on future pregnancies. Choice is being able to consider all the information in relation to your own individual situation/ beliefs/ personal history, allowing time for you to make a rational decision. Choice is having balanced open informative discussions feeling that your decisions are supported and not judged. There is no ‘we are just going to’ or ‘we will’, choice is the individual making the decisions.”
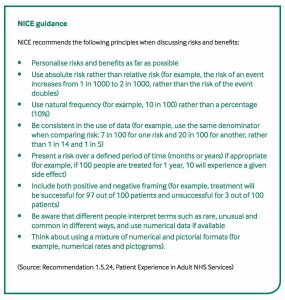
We were reminded of nice guidelines for discussing risks and benefits and also CHOICE top tips for maternity care providers.
Another really interesting point was raised about choice,
“In some circumstances there are no choices, and support needs to be given to those mothers who have had their choices limited or removed.”
Sometimes we may have no choice, in that due to circumstances beyond our control we may have to give birth or accept a situation that is far from the choice we would have made or choices have to be made for the wellbeing of mother and/or baby.
“Following my daughter’s death I have questioned the decisions we made many times wondering if a different choice may have meant she’d lived. In my subsequent pregnancies the feeling of responsibility to make the right choice has at times overwhelmed me and made me very anxious. In lots of ways I’d have preferred to have just been told what was going to happen.”
It was also raised that choice means accepting the consequences of the choices we make, both as staff and as families. Sometimes this can mean impossible questions that may never be answered.
“Sometimes we are given the illusion of choice. How information is presented is so important. Manipulated or coerced compliance can be made to look like choice. Yet, within maternity services, it’s hard to challenge this. Some caregivers reveal their own opinions in how they phrase information – about whether induction, or cs, or epidurals have risks, for example. This sometimes is presented differently to data about home birth, or vbac, or physiological third stage.”
What did become clear was choice must be Clear, unbiased, informed and not an ‘illusion’. That families didn’t want those responsible for their care to manipulate information or data to coerce a choice that they felt was right. Instead information given should allow for families to make choices that were right for them.
Yes when it came to choice, it was evident how important this was to a good maternity experience.
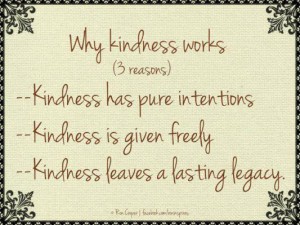
Kindness
Next we chose kindness. While many things matter during birth, simple acts of kindness can leave lasting impressions and mean so much.
“True kindness is something you give without expectation of any kind of return, not even a thank you. It’s instinctive and comes from the heart and will always benefit another heart. You don’t have to touch, smell, see or hear it but it can awaken your senses and light up your soul. It’s something that both the giver and receiver benefit from.”
“Kindness to me also includes understanding- even if you don’t make sense or or thoughts are irrational. It’s such a confusing time, someone being kind and saying ‘it’s ok I understand’ means the world.”
“Kindness is SO important. I have met many kind midwives and each time a small gesture has been performed it has meant so much. I will never forget the midwife who made me a cup of tea in the small hours after Luka was born. I was literally (emotionally and physically) broken and her kindness fixed me up enough to carry on.”
“In order to be truly kind one needs the time to be kind. How many people are in such a hurry during their day, under too much pressure or thinking of the next job, to afford true kindness? Kindness means kind words but it also means listening, accepting & acting on the kind thoughts. If you see a person in distress, true kindness is actively easing that distress both verbally and practically.”
“Kindness should be in everything we do. We should treat all women with kindness because it’s the small things that matter too. Even the most difficult, hard and situation can be made a little easier when we are shown kindness. People remember kindness and if we truly seek to show kindness it will affect how we care for women. I believe it should be one of our inner values that we keep and not allow the culture to eat away. It costs nothing and yet can have the biggest effects.”
“Kindness is being empathetic and showing the person that you understand how the person is feeling and showing that you care and that you understand.”
“A quick Google search says “Kindness: the quality of being friendly, generous and considerate.” Generous is an important one. To be kind, in my opinion, means to give of yourself, to do something that takes a bit of extra effort. To deliver a home cooked meal to a family with a new baby is kind. To offer to take baby for a buggy walk whilst mum has a nap is kind. To make a busy parent a cup of tea is kind. To be generous with your time and your abilities is kind. As for “considerate”, this is the one where language is important. Consider what language you are using and the impact that can have on a person. Speak with kindness, aim to boost a family’s confidence and pride rather than to leave them confused or with feelings of inadequacy. Consider how you would wish to be treated in the same situation. Consider what you know of the family and the impact those things might have on their experience.”
So kindness was a valued part of maternity care and many expressed that kindness had made a real difference to them, however small the act.
It was also raised that it is important to also show kindness to those who care for women.
“As families we must not forget that there are times for us to be kind. To be friendly or at least polite. To drop off a box of chocolates on the ward to say thank you. To donate some items to the hospital. To raise money for units that have cared for our children. If we have been fortunate enough to receive kindness we should remember to pass it back or pass it on.”
Yes Kindness in words and deeds really does make for a good Maternity experience for all.
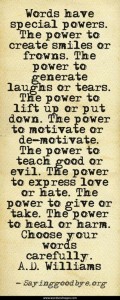
Language
Language is something that is discussed a lot in Matexp, and something that is very important to so many. Language has the power to build up, encourage and empower or to tear down, increase doubts and intensify fear. The words we use can leave lasting impressions.
“Language sets the tone for every experience. What is said, translates into what we hear and that affects how we feel. Being told I was 2-3cm and could go home if I wanted to it was ok. But what I heard was, I’m a failure, I’m not progressing, I’m wasting everyone’s time. It didn’t matter what was said to alleviate those worries, they were now engrained. Also, the word normal is a horrible word and should be replaced with various other descriptive words that can resonate more with the mother. Language is communication, understanding and respect.”
“Language is about reducing the distance between provider and parents and creating a collaborative ‘us’ rather than ‘them’. It’s as much about listening as talking, and it’s about choosing words that come from kindness, even if we can’t avoid the risk that they’re not always received that way.”
“It’s not just the words themselves (although these are important!) but also how it’s delivered. Positive phrasing is important we need to ban certain phrases IMO! A big cultural shift around certain stock phrases is needed. It’s about having a two-sided conversation/discussion in relation to decision making ultimately with the individual involved making the decision with all the facts available, I.e. looking directly at a person when talking, hello my name is campaign, doing admin once individual left room rather than spending lots of time looking at screen or doing paperwork etc.”
“For me language and the way we use language can convey so much. It should always be used in a kind way mindful of the person and their situation. Listening is so important as is thinking about the words we use. Our language should convey that we care, are interested, want the best for that person and that we are genuine. It shouldn’t be harsh or critical or brash.”
“If you can’t say anything nice, don’t say anything at all. Don’t fill silence with platitudes. Judgement is implied in so many statements unwittingly uttered when they fall on the ears of person who is suffering / has suffered a trauma. Instead hold a hand, mop a brow, smile, rub a shoulder but be so careful. It’s easy to say “well you are mum now you’ll put your baby first…” wh
en a new mum admits she feels awful, it’s said without malice, as a statement of fact as you see it BUT to the traumatised mummy it can say something different. To me it said “selfish mum, thinking about yourself, crap mum can’t do it” and so I hid how bad I felt and went home with retained placenta and developed sepsis. Think before you speak.”
“Words need to: be positive, encouraging, soothe, be honest, kind, compassionate, open, have empathy, be professional, clear and simple and always respectful.
 Words without:
Words without:
Attitude
Contempt
Judgement or jargon
Chat ‘with you’ not ‘to you or above you’
Words should not be dismissive or exclusive
Words of kindness always…Words are but leaves, deeds are the fruit.”
“The words we use provide the framework for our thinking. I can tell by the words you use what you think and therefore feel about me. Language is about communicating. We need to develop and agree a shared language to do this well. I don’t really care what your “correct terminology” is unless we have established what it means to us in this relationship. If you are not sure what words to use let’s talk about it. It’s a great way of building trust.”
“Language for me is one aspect of communication and facilitation and if we use it with the aim to facilitate then we are on the right track- this means personalising for atmosphere, experience, individual on a moment by moment level. And we must match the language with all other aspects of communication otherwise it is hard for women to trust in us as the words we use seem at odds with body language etc. Language should be used to empower, inform, educate, provide choice in a non judgemental safe, exploratory non defensive manner. That is the ideal. Consent, not coerce, create chances for inclusion in the care relation ship and take care in the words we choose- as said above we all take things in different ways, but if we are authentic in what we say then that’s a good start.”
Two words in particular that came out as needing to be thrown into room 101 and these were;
“Failure“ and “incompetent”
Language is a very important Heart Value. We need to think about the words we use, but also the way those words are used. Language can greatly affect birth because words are so powerful.
Respect
We would think that respect would be an obvious part of a maternity experience, but sadly many women and staff say they feel it is lacking.
“To me respect means an absence of any type of prejudice. It means getting to know the individual, not treating everyone the same. Acknowledging the family’s history, experience and their knowledge and understanding without making assumptions. Respecting the mother’s decisions as much as her body.”
“Respect is valuing people and listening to/valuing their opinions even if they differ from yours. Finding a way to use these collaboratively when making plans. This respect should go both ways too, no point looking for respect if you’re not giving it.”
R … Respect
E … Every one’s
S… Sensitive soul
P… We are just people
E…Eager to do our best
C… Careful how you say things
T … Two way communication needs kindness & respect.
“Due regard to the feelings or rights of others is where respect really hits in #MatExp. We must give due regard to the feelings and rights of families, whatever our personal views or experiences.”
“Avoid harm or interfering with” – another crucial one. Sometimes these feel mutually exclusive in some areas of #MatExp – can we avoid interfering with mothers and babies but still avoid harm? If in doubt, we go back to respecting the feelings or rights of others. And of course we have to consider whether the baby has rights as well.”
“Respect is valuing the person’s point of view and valuing them as a person. What they want, what they feel and this should be discussed with the woman. Actually to define respect is not that easy. I was thinking how the medical profession has commanded respect and still does and it is very aligned to value.’
“Based on my personal experience, respect is knowing and understanding that this is MY body, MY pregnancy and MY baby NOT yours (health practitioners); hence LISTEN to me, give me OBJECTIVE information to help me to make ‘INFORMED’ decisions and FIGHT/ADVOCATE for my wishes. Don’t give me your opinion if I haven’t asked for it and recognise my birth doesn’t fit round your schedule but the other way. And everything everyone has said so far.”
Respect also encompasses staff and the environment they work and care for women in.
“The first part is the respect I hope all birth professionals command, as they are doing an amazing job.”
“Agree to recognise and abide by”. Do all of the guidelines and protocols in your hospital or birthing centre command respect? Do you respect family’s birth plans? Do families respect your recommendations? Can all of these things be married together? Respect encompasses a huge amount of concepts. We all want it and we’re often slow to give it.”
“It also means respecting each other as staff, working as a team and supporting each other’s roles. Respect also included speaking up when we see wrong attitudes or treatment. It also means the respecting of other view points and realising we can all have different perspectives and that’s ok.”
Respect for women, their families, beliefs, choices and needs MATTERS. Staff too need respect for each other and but also afford respect for the amazing job they are doing.
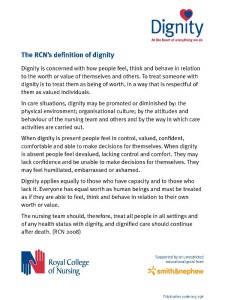
Dignity
How can we respect a woman’s dignity in birth?
“For me dignity means, allowing me to make decisions without health professional over riding them and making you feel as though you’ve said something wrong.”
“For me respect and dignity come hand in hand. Whatever happens if you have treated me with respect I will be able to preserve my dignity. Labour and birth put you on a very vulnerable place and being respected means whatever procedure or conversation takes place involving very intimate issues, I will feel like I am a human being rather than a problem or hinderance, or worse still, like there is something wrong with me, which is my fault, not a result of the circumstances.”
“Dignity is treating me in a way that doesn’t make me feel I’ve outstayed my welcome on the maternity ward.”
“For me, dignity is about human rights, and human rights are about being treated with respect…a pregnant woman or a woman in labour is entitled to her human rights being respected at all times, and she is entitled to be treated with dignity…there!”
“Recognise that respecting privacy, DIGNITY and autonomy is not an addition to care provision, but an integral part of good care…”
“Being spoken to as a competent adult rather than a naughty child, people introducing themselves before touching me, people remembering I am a person not just a uterus on legs.”
In fact this summed Dignity up perfectly.
Compassion
Last of our Heart Values, but by no means least, is Compassion. Some would argue that compassion alone is the single most important thing we can shown women in a maternity experience, if all care is based on compassion then it will encompass all the other Heart Values.
“To me compassion is seeing a person, realising that they are in need of not just your medical care but your emotional support, kindness and often just to know you actually care. It involves thought, as it can be such little things that make a difference. Think, if this was my daughter or sister how would I want them to be cared for ?”
“Compassion to me is always about time, the extra couple of seconds to smile at someone who looks worried; the couple of minutes to listen to someone who has a question or to ask someone who looks lost on a corridor if they need help; right up to the tasks that take a lot of time.”
Do we see compassion in maternity?
“When I was very sick waiting to have Joseph no one had any time to just sit with me, so the staff got a student midwife to sit and hold my hand. I’ll never forget her kindness. So even if there is no time sometimes there is another way.”
“I was really surprised when I was critically ill. I had a midwife refusing to leave as I was so poorly, she made sure she was my midwife 3 nights in a row. I had so many hugs from so many doctors, midwives, health care assistants I can’t count. I had my 27 weeker in an LNU rather than a Level 3 and they pulled out all stops so we could be cared for close to home.”
“One of my favourite consultants wasn’t even one of mine. Every day he would see me going to Joseph (over ten weeks) and give me a hug and tell me what a lovely mum I was. He was a huge support to me and probably had no idea.”
“For me, it was when one of my consultants told me “your baby *will* be premature”. I started to cry and she put her hand on my arm. It was such a human touch and I was so grateful. But I’m guessing that’s generally not encouraged, whereas for me, it meant so much: it said, I understand and I know this is hard. For me as well, it was when I finally left the hospital and one of my midwives gave me a big hug.”
“It was the array of midwives who looked after me for 10 days talking to me and making me feel almost as if I was just in a second home (ha I was in for 2 weeks which felt like a long time).”
“It was all the consultants who I had come across, always stopping when they saw me to ask how I was and how baby was doing. It was consultants who came to find me the next day to see how I was doing post c sec.I didn’t really expect that, as they must all be very busy people, but they never gave that impression of being in a rush etc.”
“I had so much kindness and compassion when I was in hospital with Joseph, my favourite was the day after Joseph was born, he was ventilated in NICU and I was in my room. I knew I couldn’t see him that day, and had been warned it would be Monday, this was Friday. I quietly crying and the obstetrician reg Charlie came in and said “why are you crying” and I said “I’m fine, I’m hormonal and still very ill and just feeling a bit sorry for myself”. He said “Nonsense, you need to see your baby and I WILL make it happen”. He spent hours organising everything to get me to NICU to see my baby, I will never forget his kindness and him realising that was what I needed, and being prepared to make it happen.”
Can we as families show compassion to staff?
“For staff I believe we should remember the hard work they do and commend them for that. Also be respectful to them. Also compassionate towards each other as a team. Help each other, treat with respect, and value each other’s gifts and abilities. Compassion I truly believe goes a long way when it comes to improving Matexp for all!”
“Immediate thought: always offer your midwife or health visitor a brew when they come to your home, coz they work bloody hard smile emoticon And we know that in the UK tea = compassion.”
“Give thanks and praise where it’s due, people are so quick to complain but never to give thanks. For HCPs, spend 1 moment before each meeting to take a deep breath, rid yourself of other thoughts and allow all focus to be on the couple/Mama you are going to speak with/assist.”
“One of the biggest revelations I’ve had this year, during a fairly turbulent time, is that it is impossible to practice compassion as a HCP towards women day in day out unless you also practice self-compassion.”
“This thread has inspired me. Tonight the children and I are going to bake a big chocolate cake and then tomorrow deliver it to the Labour Ward as a thank you to all the exceptional midwives who work so hard there.”
So those are our six Heart Values. These values are the heart of Matexp, they permeate the actions we make to improve maternity services everywhere.The Values will continue to grow and expand as Matexp does too.
Thank you to everyone who shared their thoughts and ideas with us. We had so many it was impossible to include every single one here, but we hope all the above comments capture the thoughts of women, families and staff.
Matexp is amazing and will make changes for families everywhere. A woman will remember her birth for the rest of her life so lets make sure we do all we can to make her maternity experience one she remembers for all the right reasons, which we can if we remember our Matexp Heart Values. Lets but the heart into Matexp.
Emma Sasaru