When I first came across Florence and Gill and the MatExp Campaign, I knew my group would have a lot of maternity experiences to provide to them. We are always discussing and sharing birth stories, and when I asked them for their feedback it came in abundance. Their stories, from all round the UK, have been passed on to Florence and Gill, and also to Jeanne, midwifery lecturer at Salford University. I have permission to share an initial snapshot with you here, to give you a flavour of the ordinary maternity experiences that are happening around the country and which, for the most part, do not get formally discussed once they are over.
The Good
This was the hardest section to find quotes for. Not, thankfully, because I didn’t have any good birth experiences to work with, but because I was looking for quotations praising the midwives. But when you read a positive birth story the midwives are rarely mentioned. They are there, and their actions are noted, but they do not receive praise for their interventions, because a positive birth story is about the mother: her experience, her actions and her achievement. Rest assured there are plenty of positive stories being shared amongst us, but in terms of positive feedback there is only a little:
“Although I ended up with a c-section after induction, pre eclampsia and gestational diabetes plus a lengthy hospital stay, I only have good things to say about my experience. At all points I felt they were doing the best for me and my baby. I loved the fact that, during my stay in hospital, when midwives asked you how you were feeding they always responded ‘bottle feeding, brilliant’ or ‘breastfeeding, brilliant’ – there was no obvious preference amongst the staff but they were very supportive of either.”
“When I got the epidural I had a lovely midwife waiting with me for the drip to work. I really appreciated her calm, kind attitude – she was so so lovely and I think the fact that it was one to one care made it amazing. I felt so well cared for. When I started to push everyone was SO LOVELY and I felt very in control. It was when they said I needed forceps I started to lose it a bit but they were still lovely even though I was throwing the F-word around a bit by now. I was transferred to theatre and started to get a bit scared, but again my midwife was very reassuring. I had a spinal block which sadly went too high and I started to suffocate. I had to have a GA and I was very frightened but seriously, all praise to the staff, they were so calm and kind. The consultant offered me a debrief appointment and I went to it about twelve weeks later – it helped me process everything. Whilst it wasn’t a great experience I feel the hospital did everything they could to help me and safeguard my emotional health following a scary time.”
“I had excellent care in my second pregnancy with the same midwife all the way through; wonderful home water birth and excellent postnatal care, including breastfeeding support. A great example of how important it is having the same person looking after you and building a relationship.”
The Bad
“While being assessed I gave permission to be examined vaginally on arrival to assess my progress. On finishing the exam the midwife said ‘you’re a good 4-5cm dilated already so I gave you a good stretch whilst I was there to speed it up.’ I had not been asked if I would like a cervical stretch. I did not give my permission for a cervical stretch.”
“Both myself and a friend progressed very quickly once the induction took and struggled to cope with intense pains that came every minute or less. Both of us had dismissive midwives who offered no explanation as to why the pain was so intense and why we could have no painkillers other than paracetamol. We were both told to go to sleep (as if!) and told that if we couldn’t cope now how would we cope when labour was established – which was terrifying! Both of us coped just fine on gas and air.”
“Breastfeeding support was rubbish. My husband showed me how to manually express milk after reading the breastfeeding book. The support workers just shoved my boob in baby’s mouth but I didn’t understand how I was supposed to do it when they weren’t there.”
“…..another midwife was lovely and kind and murmured comforting words as she fixed the belts and monitoring equipment, then left me behind the screen. Bossy midwife then came along and yanked back the screen, announcing that she ‘liked to see her ladies when there are being monitored.’ So I was sat with my jeans so low that my pubic hair was showing, my whole bump exposed, while a couple of women I didn’t know and their partners tried to look anywhere but at me. I had very little shame by that point but this upset me. It felt like punishment.”

“With my 4th baby I was still keen to have a homebirth but requested a growth scan near my due date to monitor baby’s size and check it would be safe [due to previous shoulder dystocia]. This was refused. They ‘didn’t do growth scans’. I could have a homebirth but not a scan. I repeated the request to other midwives but nobody suggested referring me or even seemed to care. I eventually found a midwife who took me seriously and referred me to the consultant. When I eventually got my hospital appointment I saw a registrar who honestly didn’t seem to know what he was doing. He said I couldn’t have a growth scan but refused homebirth in case I had shoulder dystocia again. After another appointment I insisted I saw the actual consultant. The consultant said I couldn’t have a scan but agreed to do a sweep 1 week before my due date. In the end, I asked about a due date induction to reduce the risk of the baby getting too big as I was so frustrated at this point and nervous of baby getting stuck again. They seemed surprised but agreed, so that’s what we did.”
The Unacceptable
Despite the draw of a catchy title, I refused to refer to any of these experiences as “ugly”. A new life entering the world is never ugly. But I feel that “unacceptable” is appropriate for these two experiences, and I hope that you do too:
“My midwife asked, whilst examining me to see how far dilated I was, if I’d like a sweep. I was in agony so I said no. She did it anyway. I screamed and hubby said he had never seen me look so pained before or since. She only said ‘done now’.”
“All going smoothly until I haemorrhaged. I was rushed to delivery and the consultants managed to stem the bleeding, with a review scheduled to decide if theatre was necessary. There was a question mark over retained placenta/products. The placenta was torn and was not confirmed as complete. I had another procedure to stem another heavy bleed with the review still scheduled for later in the day. A junior consultant came and decided that they weren’t going to take me to theatre that day despite still having heavy bleeding. I had not been given any food or drink (other than water) since the previous evening. This was 2pm on Saturday.
After this, I didn’t see a midwife (nor anyone else) for hours. My room had blood covered surgical instruments left on the side plus the swabs etc from the procedures, my catheter came out and I was left in a soaked bed for what seemed like a long time plus the bleeding was still very bad. My buzzer was not answered for long periods of time. I was eventually transferred to a ward at around 8pm. Once on the ward, I continued to bleed and clot heavily. The midwife said this was normal. My obs were low but I didn’t want a blood transfusion unless absolutely necessary. There was no further mention of retained placenta/products and I was allowed home after 3 days.
This resulted in four and a half weeks later being rushed to surgery to have the retained products removed. This was after 3 separate haemorrhages which again the community midwives said just needed monitoring. I was lucky that I didn’t get an infection. The advice in A&E was that I should have called an ambulance.”
I have a lot more #MatExp feedback to share, too much for one blog post. I will put up more soon. For now I will leave you with this illustration of the discussions at a recent Families & Midwives Together Conference I attended at Salford University:
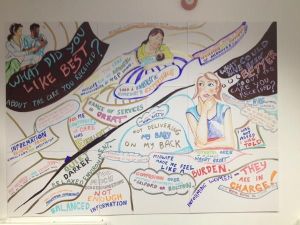
What could have been better about the care you received?
Helen Calvert. 2015

