There have been some fantastic conversations taking place on the #MatExp Facebook group, with lots of ACTION threads being posted to generate discussion. The aim of these discussions is to identify ways that we can ACT to improve maternity experiences. Big, long-term actions that might require system change or a change in culture. And small, immediate actions, that professionals and individuals can take today to improve the maternity experience of those around them.
One of the discussed topics was Tongue Tie’s, the effect they can have on feeding, but also the struggle to access help and support. So what is a tongue tie? How does it affect a mother and her baby? What can we do to ensure families access the support they need?
“Tongue-tie (ankyloglossia) is when the string of tissue under your baby’s tongue called a frenulum, which attaches their tongue to the floor of their mouth, is too short or tight. If your baby has tongue-tie, it can affect the tongues movement, preventing it from moving freely, this can cause problems with feeding, either at the breast or a bottle, speech, and moving on to solid food. Tongue tie can vary in degree, from a mild form in which the tongue’s movement is only slightly impaired, to a severe form in which the tongue is completely fused to the floor of the mouth. Feeding difficulties may arise due to the inability to move the tongue in a normal way and therefore impacting on attachment, sucking, making a seal and removing milk effectively. Many tongue-ties do not require treatment. However, if the condition is causing problems with feeding, surgical division of the frenulum can be recommended and carried out as soon as possible. It is important that families receive support from trained people as not all tongue ties can be clearly seen and each mother and baby will be different.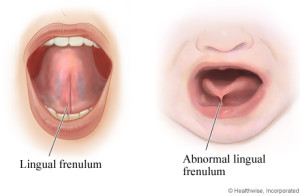
How does tongue tie affect a mother and baby? If a mother is breastfeeding tongue tie can affect latching to the breast, in fact some babies are completely unable to latch. It can be difficult for the baby to make a good seal on the breast or maintain the latch during a feed. The results can be sore nipples for mom, static or loss of weight in baby due to poor milk transfer, this in turn can affect milk supply and maintaining breastfeeding. Some babies feed inefficiently for a short periods of time, get fed up, fall off the breast asleep and exhausted, and then wake an hour later as they are still hungry, so that they are feeding almost continuously. Continuing to breastfeed can become almost impossible with the constant feeding, sore nipples and effect on supply. Babies can become exhausted, and so trying to feed becomes more difficult thus affecting the health of the baby.
With bottle-feeding babies, tongue tie makes it difficult to make a good seal around the teat. The suck is inefficient, and the feed can take two to three times longer. As the seal is leaky, babies will often dribble milk in varying amounts, thus not getting a full feed. As the milk leaks out, air can get in and is swallowed. Both breastfeed and bottlefed babies can be very ‘windy’ with the possibility of increased colic and irritability.
So Tongue tie can have massive consequences on both breastfeed and bottlefed babies. For breastfeeding moms it can mean the end of their breastfeeding journey can can affect their emotional wellbeing too.
So the question raised is, how can we support families and improve services for babies with a Tongue tie?
From the discussions on the Matexp facebook page there were three clear areas that were highlighted.
1. Clear pathways of care. Many commented and shared their experiences of lack of support. There seemed great differences in support available from area to area and it was not always clear where or to whom mothers should be referred to for assessment, diagnosis and division of tongue tie. Some commented that perhaps it should be part of the newborn checks for babies, while others discussed the wisdom in waiting a while to see how feeding progressed before doing a division.
Either way, what was clear was the need for all areas to have a simple, clear pathway to help families get the support they need.
- These pathways should be known by all including breastfeeding support workers, midwives, health visitors, neonatal nurses, paediatric doctors and G.P’s, as well as parents.
- The pathway should include trained staff to assess, diagnosis and divide tongue ties.
- That there should be support post division for feeding.
- Joined up working between private, NHS and voluntary organisations.
- Actual acknowledgement of the effects of tongue tie, something some parents reported they did not receive.
2. Trained staff . Many of the comments reflected the fact that there seems to be little in the way of trained staff to assess, diagnose and divide tongue tie. Many reported that despite problems they were told feeding was going well and getting checked for tongue tie was difficult. Some reported having to pay privately for both the assessment and treatment, as there was no one trained available in their area. Others commented on confusion between healthcare professionals regarding the signs of tongue tie and its impact on feeding, some commented that they were told that the tongue tie needed to be cut without any assessment. Also even when tongue was diagnosed many said they faced long waiting lists with no help to support feeding or maintain lactation. In areas where there are no trained NHS staff, there is no where to refer families to and so the only option is private care which has led to often a costly private market which many families are unable to afford.
So what actions were suggested?
- All areas to have trained NHS staff to assess, diagnose and divide tongue ties.
- Working together of NHS and private care to support families, provide services, if there is a lack of trained NHS staff.
- Staff trained on what a tongue tie is and the signs, effects, it can have on feeding.
- National recognised, agreed method of assessing knowledge, skills and training.
- Regular weekly clinics to keep waiting times down.
3. Support. By far the biggest number of comments were about support. Families commented again and again about the lack of support for tongue tie. There was a big discussion regarding definition of roles, appreciation of roles and how this impacts on support given. Many felt they received more support from voluntary support roles than health professionals, but then found that support limited or not not valued. Others said they received no support at all which resulted in loss of breastfeeding relationships. Others said that due to lack of support with breastfeeding, tongue tie became the issue that everyone ‘hung their hat’ on as a magical quick fix but then were left with no post division support and felt left alone to get feeding established. One mum said she ‘wished someone had just listened’ because she knew feeding was not progressing ok.
So what actions came forward regarding support?
- Always listen to the mother, if she feels something isn’t right remember she knows her baby best.
- Full assessments of feeds by qualified staff to see if feeding is affected by tongue tie.
- Information and awareness of the signs of tongue tie for HCP’s, and parents.
- Support with breastfeeding is essential as often support to position and attach baby well can be enough to improve feeding and prevent the need for division.
- Support for families who bottlefeed on ways to improve feeding pre and post division.
- Parents need information and support to make an informed choice as to whether to have a tongue tie division.
- Post division support with breastfeeding and follow up.
- Help to support lactation, pump loan.
- Specialist support for premature babies with tongue tie.
- Appreciation of roles in both the NHS, private and Voluntary sectors. All working together to provide integrated care for families.
- Clear definition for families and HCP’s on roles, who can do what and who can offer support.
Tongue tie can be a difficult issue that families face, accessing support, finding information and getting lost in the system can leave them feeling frustrated and let down. Of course we all wish we had a magic wand to instantly provide clear pathways, much needed training and support and also weekly clinics that enabled those that needed tongue tie divisions to be seen as soon as possible to lessen its impact. However, while at present support varies from area to area, what can we all do to help make changes to help families?
- Write to your local MSLC, head of midwifery, head of health visiting, PALS, commissioners or NHS trust and tell them both your struggles to access help but also when you have experienced great support.
- We can also build on good existing services or use these as a model for setting up services in other areas.
- If your a HCP and suspect a baby has a tongue tie but are not trained or unsure then signpost or refer the family to someone that is. Find out what is available in your local area.
- If your a parent that suspects your baby has a tongue tie and isn’t feeding well, seek help and keep on asking! Research tongue tie for yourself so you can make an informed choice and remember is not a quick fix but feeding will take time to settle and adjust after division.
- As support workers, breastfeeding counsellors, IBCLCs, healthcare professionals and NHS Trusts let us all listen to families and work together to provide them with the care, support and services they need, to give their little ones the best start we can.

Tongue tie support http://tonguetieuk.org/network/
Emma Jane Sasaru

Lucia Ciampa
22 July 2015 at 9:29 am (10 years ago)My son’s severe posterior tongue went undiagnosed until 5 weeks. I paid for his first division, as he was unable to feed well enough at the breast and could not bottle feed at all. We were syringe feeding him and he was in terrible distress. Despite 5 tongue tie divisions, he required feeding via an NG Tube from 2 months to 14 months. Today, at just over 2, he still has a lot of difficulty eating solid food and frequently refuses to eat. We have had an extremely difficult time accessing support. My one hope is that lessons will be learnt from this and other babies will get better treatment, diagnosis and support.
Laura
6 August 2015 at 1:15 pm (10 years ago)I agree completely – service or dealing wth tongue tie are woeful. My daughter was born in 2012 and was diagnosed with tongue tie in the delivery room. It took 10 agonising weeks of breastfeeding (bleeding nipples etc) to finally get it revised. My son, who is now 11 weeks old, was also diagnosed at birth. I was told nothing we’d be done unless it affected feeding. Well, lol and behold it did, but when I got a referral from the GP, I rang the hospital to chase it up and was told that it would be a MONTH before our details were even put onto the waiting list!. How many mothers would just give up breastfeeding completely? We ended up paying to have it done privately, and are lucky to be in a position where we could afford to do so, but this system is failing new mothers and babies.