On Wednesday I attended the NHS Expo in Manchester as part of the #MatExp team. During our session a few of us stood up to explain what the campaign means to us. My personal bit went as follows:
It is this combination and collaboration of so many different people, from across the maternity world, that makes #MatExp so exciting to me. So many conversations are being had within established communities – midwifery conferences, positive birth groups, obstetric organisations, mother & baby groups, but with this campaign these communities are coming together. And as I say, we are not shying away from the difficult conversations.
With this in mind, I decided to broach some subjects on the #MatExp Facebook group that could be considered “difficult”. I was unsure with which to start, and then this tweet from Emma Sasaru launched a conversation this morning and I just went with it.
What has followed today has been a thought-provoking discussion that has challenged many of my assumptions and made me change my mind more than once. As with the best discussions, I am still not sure what my conclusions are but it has given me new perspectives. The original question posed was:
The blog posts I refer to are Sheryl’s birth story on my own blog, and Southwark Belle’s piece entitled “Normal Not Normal“. I then went on to observe that when I hear the phrase “normal” birth I am imagining that people simply mean “vaginal” birth. Is it as simple as that?
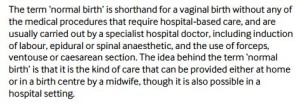
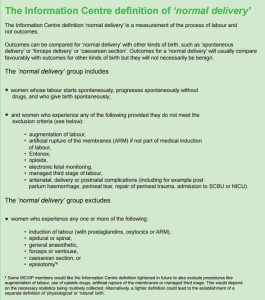
Well no, no it isn’t. It quickly became apparent that there are a couple of definitions of “normal birth” available. One group member explained that “Interestingly, one of the first definitions of normal birth came in 1997 from AIMS, the radical women’s organisation, who defined it as ‘a physiological birth where the baby is delivered vaginally following a labour which has not been altered by technological interventions’. So this was a movement that was led from a women’s organisation to counter the over-medicalisation of birth.”
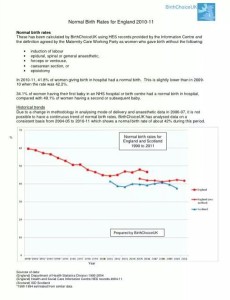
And from this 2010 publication:
And from this in 2007:
It seemed that the word “normal” had specific meanings for groups researching and monitoring maternity outcomes, and that this was a discussion that had been had many a time. Indeed, Sheena tweeted this morning
So why is it such an important and emotive discussion? Well because we have learned time and again in #MatExp LANGUAGE MATTERS. Words have huge power and different people understand things in different ways, depending on their experience, perspective and knowledge of the subject in hand. Declaring that some types of birth are “normal” begs the question what are the other types of birth then? And if the opposite of “normal” is “abnormal” are we comfortable telling women that is how we define their experiences?
It was clear that for many women the term “normal” is perceived as carrying a value judgement. It is not simply a medical or scientific definition, it is a statement about them and their experience that allows for feelings of failure and inadequacy (as with so much to do with the massively emotive subjects of maternity care). Comments included:
“where I work in a different area of healthcare, it’s understood that everybody’s normal is different, my normal vary vastly from your normal, but there is a range of normal we would expect that to be in. Having babies is different imo because you are doing something you don’t do very often so it’s difficult to define your ‘normal’ and where that might fall on the large scale of normal within birth. It can lead to people feeling inadequate.”
“the feeling of doing it wrong, not experiencing a normal birth can put people off a second time. A friend of mine is terrified because last time it all “went wrong” and she’s adamant that she won’t get pregnant again unless she can have an elective section because her body can’t do it properly.”
“Who has set the definition for normal. How do we know what normal is? How did women birth 20, 50, 100, 1000, 5000 years ago? What about culture? What is normal here may not be normal in other lands, races etc. Normal is an awful word because it gives the idea everything else is abnormal so therefore not right or not as good or missing the mark. But that is harmful label to add to a birth experience for many many reasons.”
“By terms such as ‘normal’ we make women believe that if they don’t attain that they have not done something they should. That in turn may make them feel they have ‘failed’.”
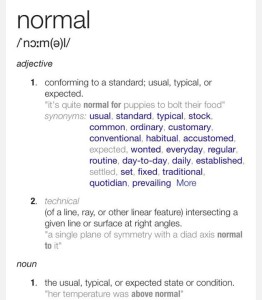
Emma kindly provided a dictionary definition of the term and observed that “its definition doesn’t relate to birth in any way”.
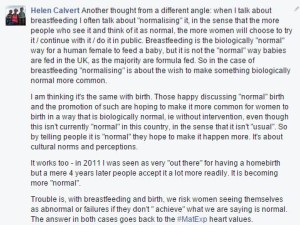
And of course there is also the fact that our definitions here do not match up. The definitions of “normal” birth explained above are not currently “standard, usual, typical or expected” in the UK as per the dictionary definition of the word.
One doula observed “Normal is the wrong word to use because right now a positive physiological vaginal birth is NOT the norm”. So is there any value in naming it as such when by a simple dictionary definition that could not be further from the truth? I think there might be, but more of that later.
BirthChoiceUK addresses the issue on their website (read the full page here) and explain that “The term normal birth is not meant to be judgmental in any way. We are instead trying to produce some measure of how much technological intervention is currently used in birth. These statistics of course do not tell us anything about a woman’s experience of birth which is likely to be of far more importance to her than whether she was induced or had an epidural or had her waters broken. It is hoped that every woman can have a fulfilling and positive experience of birth regardless of the interventions she has received. This is, of course, much harder to measure!”
And where does birth trauma come into all of this? What of the women who have had negative experiences of birth? What can the word “normal” possibly mean to them? And for those women who have had a “normal” birth as defined by the NCT and AIMS, are they still entitled to feel traumatised if their experience was not a positive one? It was discussed at length that so many apparent problems with the language come from individuals conflating the words “normal” and “positive” but throughout society we find people and cultures who believe that the two are one and the same thing. “Normal” is a generally positive term, meaning good things, which is of course a whole discussion in itself. Nevertheless it is easy to see how a woman with a negative birth experience will not thank you for telling her the birth was “normal”, and how a woman who has had a positive experience will be unhappy with the idea that hers was not a “normal” birth.
So apart from the need to gather statistics across maternity units, what other uses does this idea of “normal birth” have? Midwife Jenny Hall was kind enough to explain “The need to differentiate what is ‘normal’ and not does come down to the legal responsibilities of a midwife. A midwife is in law able to care for women without other health professionals until the process moves into areas outside the boundary of ‘normal ‘. She then legally has to refer to someone else for assistance.” There is then an important legal issue here, and other birth professionals on the group emphasised that for them the term held no value judgement at all:
“I think of normal birth as a spontaneous vaginal birth with no intervention at all, but I’m a midwife and we use these terms as classifications rather than attributing any value to them…… When I talk about normal I’m not using it in a judgemental way, just descriptive, but I am mindful that many find this term difficult.”
Yet throughout today I have had the creeping suspicion that two of my viewpoints don’t match up. I was questioning the use of the word “normal” for a maternity experience that is how human females have been designed to birth their children, yet I am constantly banging on about the need to “normalise” breastfeeding. An uncomfortable feeling of double standards was edging up on me. Giving the whole subject a bit more thought, I commented:
For the #MatExp “heart values” please read Emma’s blog post.
This angle is well articulated by Professor Soo Downe in her interview with midwife Sheena Byrom:
Miranda Dodwell of BirthChoiceUK was keen to emphasis the historical perspective: “having been working on the ‘normal birth’ agenda since about 2003, I realise how far we have come to be having this debate.” She recommended further reading in the shape of Practising childbirth activism: a politics of evidence “about the importance of introducing the concept of normal birth in terms of childbirth activism in driving change.” However, she and others were happy to discuss the idea that it may now be time to move on from the concept of “normal birth”, despite “the power it has had in creating a change of perspective towards women’s experience of maternity care“.
If we are to move on from this terminology, what are the alternatives? Both in terms of new words and in terms of new approaches? There were a number of suggestions from birth professionals:
“Unassisted birth would probably be closer to the mark but the meaning is associated with ‘free birthing’ these days. l guess for me ‘normal’ could be what the woman was expecting and not our version of normal.”
“When I hear the ‘normal’ discussion and how heated it gets I don’t have a satisfactory alternative to the word ‘normal’. Physiological?…bit of a mouthful and a challenge to spell. Vaginal? Many struggle to include the word vagina in general conversation so possibly unacceptable?”
“Rather than focussing on ‘normal’ l tend to look at how satisfied the woman is with the outcome. It’s her birth so she should define it.”
“I tend to use words like ‘physiological’ and ‘needed help’ or ‘complicated by’. Rather than normal, which has different connotations.”
“I use SVD (spontaneous vaginal delivery), assisted (instrumental) delivery or Caesarean”
And from parents:
“From the point of view of mums talking to each other about their births… I’d say ‘normal’ is too vague, fairly meaningless, and not generally used. ‘Natural’ is used a lot.”
“‘Physiological’ may be technically correct, but sounds so much more excluding than a two syllable simple Anglo-Saxon word. ‘Natural’ also has a lot of judgemental baggage.”
“Personally, I think maybe the accessibility of the term normal is what’s become problematic about it? ‘Physiological’ seems more medical, so perhaps using this term would prevent women feeling judged?”
But as you can see consensus was hard to come by. Amy Prodgers (@BirthSalford) summarised, I suspect, the feelings of many in the discussion:
As a possible, and remarkably simple, solution, one of the group’s midwives suggested “Why not use the term birth? And let the categories be an additional ‘box to tick’ not together with ‘birth’ am I making any sense??? So ‘birth of baby boy’ (male infant etc etc) then tick, vaginal/forceps/water-pool/home/hospital and so on and so on) – the word birth describes the event – that’s exactly what took place #languagematters. It’s just habit in maternity services, it could easily change – the hospitals/birth centres/ organisations etc could still get the much needed figures”.
Southwark Belle furthered this thought “I think we’re now at a stage where defining one set of choices/circumstances as ‘normal’ / best and using that to set targets just risks swapping one dogma for another. I much prefer treating it all as birth and each intervention individually rather than lumping a whole lot of things in together.”
So is birth just birth? Each instance its own unique set of circumstances and experiences? Can hospital notes and databases possibly be built with this in mind? Can statistics be gathered on this basis? Does the biological, historical way of giving birth need to be normalised to the benefit of families or are all modern options equally valid and ‘normal’?
This comment stands out for me, from Seana McCoy Talbot (an NCT volunteer who is standing for election as NCT President):
“Our starting point always has to be compassion and empathy, but also to know the evidence.
It’s instincts plus knowledge.
Heart and head.
Art and science.”
@HeartMummy 2015





MelBT
5 September 2015 at 9:36 pm (10 years ago)Following the birth of my first child, I had to take her to a clinic as she had talipes. A doctor asked me if I’d had a “normal birth”. Yes, I replied, then he corrected me saying, “oh hang on, your notes say a c sect” I replied saying “yes, and that was normal for me, as it’s the only birth I’ve had”. The nurse working with him gave me a big grin! Language matters!
Carolyn Hastie (@CarolynHastie)
6 September 2015 at 12:51 am (10 years ago)This argument has been raging for decades.
A response in the 80’s to the debate about birth terminology and what’s ‘normal birth’ mean was that ‘normal is a setting on the washing machine’.
Each woman’s experience is uniquely her own.
Calling the birth of a baby ‘birth’ and then the mode if required e.g. paper work is a sensible way of eliminating the emotional cues and hooks, including that dreadful sense of ‘failure’ for not being ‘normal’.
Sarah Davies
6 September 2015 at 7:00 am (10 years ago)I run an Evidence Based Care for Normal Birth module – and every semester have a discussion with the midwives about what to rename it. We’ve thought of ethical birth & positive birth but neither of these convey the in-depth knowledge of physiology/ psychology covered in the module or the range of midwifery skills that are needed to support the finely balanced hormonal processes of birth. Maybe just Physiology & Psychology of Birth. Ideas welcome! Perhaps important to remember that historically midwives attended all births, and twins, breech births at home but around the 1902 act in the UK, when midwives were given professional recognition, the role of caretaker of normal birth was given to midwives by doctors in order to relieve them of ‘ the tiresome and unremunerative work’ of looking after straightforward births. (I’ll find the origin of the quote). Then midwives took on the mantle of experts in normal birth – so ‘ normality’ is a word that was useful for professional boundaries rather than any description of womens experience. It is such a loaded word especially because its opposite is ‘abnormal’ – in a culture which tends to think in opposites, this is really unhelpful – and in fact there are many shades of normality/abnormality as people have pointed out. This debate links with the categorisation of low and high risk – again, not helpful. If we move to a continuity of midwifery care system for all women – where midwives / women consult obstetricians when necessary, perhaps the whole normal/abnormal debate would become less relevant. As Becky Reed from the Albany midwifery practice always said “we have an ‘all women’ caseload”.
Catherine Williams (MSLC rep, NICE lay rep, nct)
6 September 2015 at 8:17 am (10 years ago)I think it is important to flag that the ‘normal birth consensus statement’ was a consensus statement – from the Royal College of Midwives, nct, and the Royal College of Obstetricians & Gynaecologists. Multidisciplinary working involving lay people as equals has much to offer – and much has been achieved in that way already. Let’s do more!
Julie Dutra
8 September 2015 at 5:58 pm (10 years ago)I just commented on one of the linked blogs in a similar vein but thought it was important enough to restate here, that I feel as a mum I do need some sort of easy word to classify all “non c-sections”. Birth alone would not be enough to describe my experience but “unmedicated, natural birth” sounds prissy!
Helen Calvert
8 September 2015 at 6:01 pm (10 years ago)How would you feel about “straightforward” or “uncomplicated”? H.x
Bryony strachan
13 September 2015 at 10:00 pm (10 years ago)Really good debate. I sympathise with banning the word normal as this implies not normal. Julia frosts article on the utopian view of birth is a great read. I like to use the word birth. In fact giving birth rather than birthing as a mother gives or gifts birth to her baby.
I would love to change the language we use to ensure every woman knows how amazing they have been in giving the gift of birth, which ever way and what ever help they have.
http://www.researchgate.net/publication/229175861_Utopian_Theory_and_the_Discourse_of_Natural_Birth
Helen Calvert
14 September 2015 at 5:46 am (10 years ago)Thank you so much Bryony, I will share that link with the group. H.x
Sheena
2 November 2015 at 10:54 pm (10 years ago)I think if the word offends – let’s try and change it. I am a great believer in language being a major influence in experience and outcomes.
Two questions:
If we use a different phrase, will it change the feeling of failure if not ‘achieved?’
Can we try to focus on enhancing relationships and supporting physiology as much as possible, no matter what mode of birth?
Thanks!
Southwarkbelle
3 November 2015 at 9:23 am (10 years ago)Replying as per Helen’s request!
In answer to the 1st question I think it would be hard to find an alternative word that didn’t suggest good/bad success/failure to many women. When so much talk and effort goes into encouraging births that meet one specific set of criteria then whatever label we put on that it will be implied that those who dont tick all the boxes have failed. Also that those who do meet the criteria but don’t feel the birth was normal or positive shouldn’t need or ask for help.
I wonder what the point of having this one set of criteria is anyway? It clearly goes beyond data collection at this point and with so many things lumped together its pretty crude for that anyway. Intended or not “normal” birth has become the ideal or indeed only good outcome for many. I would rather we just call it all birth and treat all interventions individually in notes where needed.
On question 2 yes definitely to enhancing relationships. What does supporting physiology mean though? I’m all for supporting women and their individual informed choices but that may involve overcoming physiology rather than supporting it for some. Perhaps what we should be doing is setting aims and goals around supporting the woman not the process?
Sally oneill
26 April 2016 at 7:20 am (9 years ago)Have done work around this so many issues came to light , the connotations of normal with anything else becoming abnormal ,no standardised definition of normal ,current practises of monitoring ,epidural and cs becoming normal practises moving normal along the continuum . Asking midwives their definition of normal was also highlighted, women’s expectations of what they considered normal was so differing individually . I would like to see normal disappear and concentrate on more individualised care .