I was asked to do a talk to student midwives at Salford University last month on the topic of “Women’s Voices” in maternity care. As part of my presentation I included the voices of the midwives who work in maternity care, and a reminder that there are many other women for whom maternity care is their professional, as well as perhaps their personal, experience. “Women’s Voices” in maternity care should cover the midwives, obstetricians, health visitors, doulas who care for us, as well as the women giving birth.
So I decided to start a series of blog posts on “Women’s Voices in #MatExp” from the point of view of those working in maternity, and this is the fourth of those. Unlike the others, this one is anonymous. You can read the other blogs in the series here:
And yes, I will be doing a “Men’s Voices in #MatExp” series too. Because this campaign is about all voices.
Helen.x
*********************
I have been a sonographer for 13 years, and I’ve asked to be anonymous because I want to be honest, and I don’t think my managers would appreciate every aspect of this.
I’ve worked in a few different NHS trusts over the years, and now work in a small, rural hospital.
I do both pregnancy and non-pregnancy scans, and enjoy the variety in my work. There are more complaints around pregnancy scans, but my overwhelming impression of pregnancy scans is that it can be very hard to meet parents expectations in the NHS.
For routine, screening scans parents generally expect the reassurance that all is well, without necessarily fully considering that the scan findings may be devastating. I have a moment with the notes (hopefully, if the mum remembered them) to quickly obtain a bit of history which may give me an indication that the parents may actually be extremely anxious- but some things aren’t written down, and I struggle to determine the body language differences between anxiety, or that I’m interrupting an argument between the parents, or there is worry about something unrelated to the scan, all while the mum may have a desperately full bladder.
Once the parents are in the room, its usually only a minute or so before the lights are dimmed, if they were ever turned up in the beginning. Myself, and older colleagues have noted how our eyes adjust more slowly to sudden darkness- I used to have no trouble going from bright light to darkness in a scan room, but now I’m older I can’t see very well when the lights go off- not very helpful for the scan, but keeping the room dim all the time adds more barriers to communication.
I have been scanning a number of years, but I only learned a couple of years ago the importance of eye contact in those first seconds of the scan. I think if I’d learned that sooner, I could have easily made more clients feel more welcome. Right at the beginning is when I’m usually checking I’ve got the right patient on the computer screen or paper details, probably staring at a screen, and I expect I really came across rushed or off-hand, before I knew better. I have asked for customer skills training, but the training I have had has been more about dealing with challenging behaviour, and when I asked for training around breaking bad news I ended up on a course which was more about end of life conversations, which was interesting, but geared to spending a lot more time setting the scene for breaking end of life news without interruptions, rather than sonographers specific task of breaking bad news very quickly, with little warning.
Something that comes up time and again, is how rude sonographers are, prodding bellies and saying how fat our clients are. I’m sure a lot of us could gain from some training in customer service, but there is a reason behind the hurtful words. A scan can be uncomfortable- pressing on a full bladder isn’t great at the best of times, but sonographers end up pressing harder on larger tummies trying to see the detail that is required for that scan. We try not to, not only because we don’t intend to hurt our clients, but most sonographers are in physical pain scanning and pressing harder makes it worse. We are our own worst enemies at times though, because we concentrate so hard on what we are looking at on the ultrasound screen. So, brains may not be fully engaged on saying tactful comments, we may not realise how hard we are pressing (I rarely notice the pain I am in until I finish up the scan, and realise I shouldn’t have pressed so hard).
At the end of the scan, the other vital part of our job is communicating the findings, which usually involves giving a copy of the report to the parents in their notes.
We have to explain what limitations there are on the scan- have I seen everything perfectly like the text books? Usually not, and then we have to explain why. I’m not aware of too many people feeling insulted when its baby’s position that is a limitation, but the various ways we say we lost detail because the sound waves were travelling further (which happens if there is a layer of fat in the way) can be perceived as insulting. I know in my trust the midwives try to mention this to larger ladies before they come for any scans, and I feel that being forwarned helps when the sonographers then are repeating something already said. It doesn’t seem too shocking if I’m trying to explain the extra layers around where I’ve been scanning have limited what I can see, if its already been mentioned, hopefully by someone they trust. Sometimes that hasn’t happened, or the parents haven’t taken it on board, and some of us sonographers manage to say things quite badly. Probably in fear of saying it badly, some of us don’t mention it all, and leave it to the midwife to explain the terms on the report, which can be just as upsetting.
Sonographers sometimes across as grumpy, and one possible reason is that we are usually rushed. My day in obstetrics is divided into 15 minute slots- with double slot for first trimester screening and the 20 week anatomy / anomaly scan (different places give it slightly different names), and a bit extra for twins. In that time we really need to allow about 5-7 minutes for trying to document the findings accurately, and producing a copy for the parents to keep in the notes (IT technical issues can easily double this, and are a regular problem where I work now).
Some scans take longer than the allotted time, and sometimes in that short time interval I have to give devastating news, try to be supportive but also find another health care professional to handle the initial grief and arrange what happens next. With no time to reflect I must carry on and scan a lady who might have been kept waiting longer, with a desperately full bladder. I try hard, but part of me is probably still processing the blow I dealt the previous lady, and hoping that while distracted/upset I am doing my job well enough for both clients, and I really hope the lady who has been kept waiting is kind, because I can’t tell her any of this.
The 15 minute break slot I get each list is rarely a break, but just a little leeway so I can try to take a minute or two extra with with each lady I meet without running too late by the end. My lunch break is officially 30 minutes, where I’d love to step outside and enjoy the beautiful grounds my hospital is in, but many days in obstetrics I barely have time to eat in the scan room, before washing my hands and continuing to run late.
I’d love to spend longer, explaining each part of the report, going into the parents particular concerns and signposting them to the appropriate person if I am not the one who can help.
Officially I need to work on my time management. I take too long, I must scan too slow or talk too much. My rescan rate is too high (at the 20 week scan, if we can’t see everything in one visit we are allowed to offer one rescan, which where I worked previously wasn’t ever counted or limited, but now I use that option too freely apparently and I must have less than 10% rescan rate), but that means I must scan for longer to see everything- it is unthinkable that I would say I had seen something when I hadn’t, but I do wonder what will happen when sonographers who aren’t as honest as I am, or feel more pressured than I do, get to this point.
I have been specifically told to talk less to parents before the first trimester screening test, because after a conversation, some mums decided against it. In my old trust we were told, as Band 7 staff in the process and the person about to do the test, that we had to be sure the ladies really wanted it- and check they have heard the potential outcomes including that the diagnostic test, with a risk of miscarriage, may be offered. Where I work now I may ask if they’ve discussed the test with their midwives, have they seen the booklet, but I must not ask enough for me to be confident about the information they have, because their community midwife takes responsibility for this.
Screening tests are an option, not compulsory part of pregnancy. Many women I meet wouldn’t dream of having a pregnancy without a scan, but its not an informed choice if the mum gets in the scan room before she realises the scan is optional-this is something that happened last week.
My personal choices around scans have changed over the years, going from wanting everything going first time around, to having none with my third. I found the anatomy scan with my second child a hugely anxious time, knowing the potential conditions that could be diagnosed, and the huge number of abnormal but unexplained things that might be seen, and of course the range of conditions that a scan would never detect.
A dear friend had a devastating diagnosis at a 20 week scan before my third pregnancy, which meant baby needed delivering at a specialist centre for the best chance of survival, and I was hugely affected by how the family were affected by the diagnosis and the stress throughout the final 20 weeks of pregnancy. Their experience and my attempts to support them made me evaluate exactly what I would gain or lose from scans in my third pregnancy, and, for me, at that time, the decision was not to have scans. The same events affected other people differently, and they tell me they wouldn’t dream of not having a scan after being involved with such a tough experience, which I can completely understand, appreciate and support. I’m not planning more children, but if I did I would have to consider it all very carefully- I don’t know if I would opt for scans or not.
In the first trimester screening scan, sometimes called the NT scan, sonographers are audited in a few different ways. Where I work we have one 30 minute appointment, and if we can’t obtain measurements that meet the national screening committees criteria, then we must offer the quad test. So, we get audited on how many ladies end up being offered the quad. We are audited that our images meet standard criteria. We are audited that our measurements fit a national expected scale- and steps are taken if we don’t meet all these criteria. It isn’t too hard to meet these criteria in a baby that is lying in the perfect position, but the position of baby is one thing outside of our control.
I imagine this scan will be around for a while yet, though I am glad to know non-invasive prenatal screening has been around in private practices a while and hopefully will become more widespread in the NHS in years to come – this blood test is a much more sensitive and specific screening tool, but it is currently quite expensive.
Something else sonographers do that causes conflict is limit the number of people in the scan room, and warn that noisy or disruptive children may need to leave. If there is an accompanying adult then they miss the scan by having to leave with the child, or the scan may be abandoned if the mum is the only adult with unsettled children. I have tried to continue to scan while a child was working very hard to stick their fingers in the fan, run around, screamed constantly, but these are situations where I have to stop before I make a mistake.
It is also very difficult to concentrate when an excited parent/grandparent has someone extra to talk to. The rare time I break the rules and allow someone extra in, I have usually regretted it. I must need further training in being politely assertive to obtain the quite atmosphere I absolutely need to concentrate on seeing all the structures I need – in the given time.
If I scan in silence, I am complained about for being too serious- so I try to keep a light hearted, pleasant line of conversation going while I stare at the screen intently concentrating, looking for potentially life threatening problems with baby. Its a situation perfect for misunderstandings.
Keeping the chatting going is much harder on those days I have a bit of a headache, or my 3 year old has had a bad night, or my 7 year old had a nightmare. I suppose I might call in sick for not being on top form, but the team I work with is so small so I know parents may turn up for long-awaited appointments and be forced to rebook, or my colleagues might try to squash extra scans in an already full list- with all the usual pressures still standing for making it a pleasant scan, not rebooking, etc. And of course, like any business, sickness records are kept and if you take sick time too often, then steps are taken.
I’m struggling at the moment. Concentrating non-stop, knowing mistakes mean huge potential consequences for families, doing it all against the clock and targets is draining me. By the end of my working week I usually feel too exhausted to cuddle my kids before I crawl into bed, unable to cook or eat tea, straight from work, hoping I can take time out of family life to recover from my week. My head hurts, I keep going faint, but the GP says there’s nothing to worry about. My sickness record is something else to worry about. I can’t cut my hours- I think I could probably cope if I were doing it less. If I could have some time for catching up at the end of my lists, I think I could do a better job.I work with a good team, but the managers don’t seem to get the pressure they are putting on us. But then, I don’t know what pressure they are under. I suspect my manager is struggling, but trying to keep it private. She is taking unpaid leave to try to keep going, but scheduling it has been almost impossible. The needs of the service come first.






























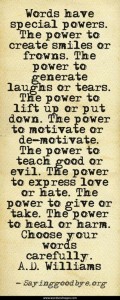 Words without:
Words without: