Welcome to the start of ‘A Catalogue of Maternity Experiences’. Rachel @enduringdelight from This Woman’s Work Blog gets us started with her positive maternity experiences and how they inspired her. We hope this motivates you to share your story too.
Read “An Important Catalogue of Your Maternity Experiences” to find out more about this #MatExp action, and submit your story.
I am by no means as eloquent when writing as some of the other members of the #MatExp community, but after seeing this tweet from the inspirational Sheena Byrom and following a suggestion from the lovely Helen Calvert I felt it really important to write this post. As Fab Obs Flo once told me, outside of my comfort zone is where the magic happens (thanks Flo!).
“I’ve learned that people will forget what you said, forget what you did, but people will never forget how you made them feel.” – Maya Angelou
This quote pretty much sums up the story of our children’s births. I will never forget how the people who cared for us made me feel and how they changed my life.
 I’m Rachel, mama to (almost) 7 year old boy/girl twins and our youngest little boy who is 3½ years old. I’m also now an NHS Breastfeeding Peer Supporter, MSLC Vice Chair and birth junkie with a particular interest in improving birth experiences for families and the relationship between attachment and neuroscience.
I’m Rachel, mama to (almost) 7 year old boy/girl twins and our youngest little boy who is 3½ years old. I’m also now an NHS Breastfeeding Peer Supporter, MSLC Vice Chair and birth junkie with a particular interest in improving birth experiences for families and the relationship between attachment and neuroscience.
I can’t even remember how I stumbled across #MatExp , but it is an amazing movement; it excites me to know that there are many other people out there as passionate as I am about supporting families to have the maternity experience they crave. For a long time I thought that my passion for positive birth and all of the issues surrounding it might just be a bit odd!! I don’t contribute to #MatExp as much as many or as much as I would like, but it is a privilege to be part of that community and so I am very grateful to some of #MatExp’s lovely ladies for encouraging me to persevere with writing this when I was struggling.
If you follow #MatExp you will know that, sadly, for a lot of the amazing people contributing to this grass roots movement inadequate care or a negative experience was their catalyst for getting involved. For me the complete opposite is true, but sometimes that makes things difficult for me because in certain circumstances it’s really hard to talk about having had positive birth experiences as I feel like somehow people may interpret that as me being critical of theirs.
A positive birth experience for me was always going to be a physiological one, but I am not militant about it and I don’t believe that’s what everybody should have. Moreover I believe that a birth that deviates from a woman’s ideal can still be positive if that woman is consulted, supported and given options rather than dictated to.
Having beautiful birth experiences and successful breastfeeding journeys are what drove me to become involved in movements like #MatExp and peer support. I’m all too aware that sadly not everybody is as blessed as I am to have had experiences like mine, but I really feel like they should be. It shouldn’t be a lottery that thankfully I won. Every woman should be listened to, respected and involved every step of the way in her own and her baby’s care.
“Do the best you can until you know better and when you know better, do better.” –Maya Angelou
My maternity experiences were very different, but positive in their own right. In hindsight there are things I would change if I could go back and there are things that weren’t ideal and that health care professionals should and could have dealt with differently, but that doesn’t make them a negative experience. In fact the only reason I know that there are some things I would change and things that could have been done better is because of all of the things I have learned since, but if my birth experiences hadn’t been positive to begin with I wouldn’t have been propelled into the world of positive birth and maternity experience and so would have been none the wiser.
The birth of our twins involved an induction at 38 weeks and 4 days gestation. I see so many negative things written about induction that it is important to me to write about this. I’m not writing about the process of induction and how good/bad this is for women and their babies. What I want to write about is the fact that, if you have knowledgeable and respectful people caring for you it can be a positive birth experience even if it is not your ideal. I am so grateful to the midwife who cared for us when our twins were born. To be honest I think she was the catalyst for my passion for birth and the person who gave me the confidence to decide on a home birth for our youngest son.
I’d had a very straightforward multiple pregnancy and so despite being classed as “high risk” (a label I despise) I hadn’t needed much care at the hospital other than routine appointments and so was quite nervous about how I would gel with midwives caring for me when the time came for our babies to be born in hospital. I need not have worried; as soon as Carmen walked in the room she came across as so knowledgeable and this gave me complete faith in her from the outset. It was clear that she had every confidence in my body’s ability to do its job which in turn gave me that very same confidence. After all, if she thought I could do it then why wouldn’t I?
Something that particularly stays in my mind is her supporting my decision to not have an epidural. I had never wanted one, but the anaesthetist was fairly insistent on me having one almost as soon as the drip was in my arm and I think I would have given in were it not for Carmen; instead when she could see the conversation was becoming too much for me she delicately stepped in and dealt with it whilst remaining respectful and professional towards her colleague. I remember feeling so grateful to her for that and so relieved to not have to fight for what I wanted.
“Drinking tea intelligently.” –Tricia Anderson
Our twins were born about 8½ hours after my syntocinon drip was started. I remember Carmen talking me through each stage of the induction; she read my birth plan and made sure that I didn’t remain on the bed and that I got breaks from the CTG trace, she got a rocking chair to allow me to be more upright and off the bed, dimmed the lights and left us to it as much as possible, but without ever being more than a stone’s throw away. She really did drink tea intelligently!! Even when she was drinking tea for real on her break I was her priority and she came back when I begged for her to.
Three years later I found myself excitedly planning a homebirth for our third child in our teeny terrace house. There were a couple of little administrative hiccups, but each midwife I came into contact with was positive and enthusiastic about our plans which made me feel really confident about our decision.
When the day came for our little boy’s birth I was blessed to have the support of another intelligent tea drinker; familiarizing herself with my birth preferences and facilitating them; Lorraine was a quiet, reassuring and confident companion and exactly what I needed. Although she hadn’t been my named midwife I had met her at a routine appointment and as soon as she arrived at our home on my son’s birthday I remembered how enthusiastic she had been about my plans for a homebirth when I had seen her all of those weeks before so I immediately felt calmed by her presence.
It was a very straightforward, if a little speedy, birth and with the aid of a tens machine, some hypnotherapy and a little gas and air our son was born in water less then two hours after Lorraine arrived and probably only about 20 minutes after the arrival of the second midwife. They stayed with us for a couple of hours or so after the birth; helping my husband to tidy up and ensuring we got breastfeeding off to a good start, being attentive, but respectful of what was an important time for us.
The midwifery team’s apparent confidence from the outset in the decision we had made to have our son at home as well as Lorraine’s confidence in her own ability as a midwife and my body’s ability to deliver our baby served to make me more determined to support other women and help them to achieve a birth experience that they were happy with. This is how I came to become involved in our local MSLC just a few months later; I wanted so much to make a difference.
It goes without saying that when mistakes are made we need to learn from them and make sure that those mistakes never ever happen again; I’ve worked for solicitors on birth injury cases and am all too aware of the devastation that can result from human error.
In addition though it is vitally important that we learn from the positive.
There are many midwives (and other healthcare professionals) who are wonderful at their jobs and passionate about the care they provide. These people have life changing positive impacts on families every single day and I feel so strongly about the fact that best practice should be shared and celebrated so that it can be replicated by others and that’s what I wanted to do today and to achieve in writing this. I wanted to share my positive experiences and celebrate the midwives who made a difference to me and to my family; I will forever be eternally grateful to you.
“We are like a snowflake; all different in our own beautiful way.” – Unknown
Most of the world faith traditions have stories of the birth of special people. There are signs accompanying the birth. Stars, wise men and phenomena announcing the arrival on earth of someone wonderful. Perhaps these stories are signs of what we should celebrate with each birth. The birth of every single child and every new parent is special.
As we welcome these little ones into our world let us think deeply. What physical environment is most fitting? What psychological and emotional factors should be named and made present? What people and attitudes will build that loving cradle of experience to welcome the newest member of the human race – our race? Every child and every mother are unique – like every snowflake.
Maternity experience is about creating the best for the newest.
I am fortunate that my experiences have been positive. Let’s always put women, children, families at the centre of our care and create experiences that reflect how special birth is.
Rachel xx
(The content of this post is my story, but a special thank you to John Walsh not only for taking the time to proof read and make some suggestions as to the finer detail, but also for his encouragement. You can read more of John’s wonderful musings here.)
~ How has your maternity experience influenced you? ~
Look out for @HeartMummy Helen’s story next month.
You can submit your story too; see the second paragraph for more information.
Like what you’ve read? Share far and wide 🙂









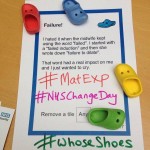

















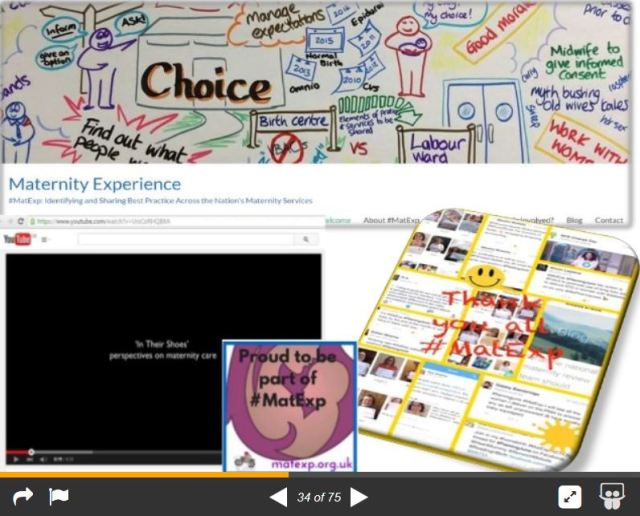






 Graphic record from our #MatExp Whose Shoes? workshop, held at Kingston Hospital. New Possibilities are the graphic artists.[/caption]
Graphic record from our #MatExp Whose Shoes? workshop, held at Kingston Hospital. New Possibilities are the graphic artists.[/caption]





